Antibodies against apoptotic cells may predict kidney transplant rejection
1. Kidney transplant patients have higher IgG reactivity to apoptotic cells (IRAC) than healthy patients.
2. Greater levels of pretransplant IRAC were associated with increased risk of allograft rejection, and were particularly predictive of antibody-mediated rejection (AMR).
Evidence Rating Level: 2 (Good)
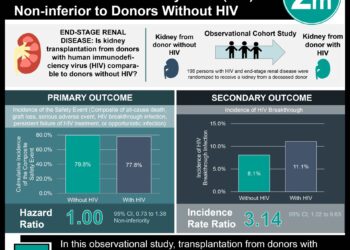
Study Rundown: While immunosuppressive therapies have greatly reduced acute cellular rejection of kidney transplants, they have not succeeded in preventing the long-term kidney failure associated with other modes of rejection. In determining candidates for kidney transplant, patient serum is often screened for predictive markers of transplant failure or success. While many studies have shown correlation between HLA-specific antibodies and poor transplant outcome, the contribution of non-HLA antibodies remains less clear. This study evaluates correlation between pretransplant IgG antibody reactivity to apoptotic cells(IRAC) and long-term kidney transplant success. When compared to healthy control subjects, kidney transplant patients were found to have higher pre-operative IRAC levels. In patient comparisons, higher IRAC predicted graft failure. Interestingly, the predictive value of IRAC for poor graft survival was only significant in long-term (> 12months) evaluations. Supporting the likelihood that IRAC plays an active role in this transplant rejection, patients with antibody-mediated rejection(AMR) had higher IRAC levels than patients with other mediators of graft loss. Particularly, IgG1 and IgG3, known to activate the complement pathway associated with graft failure, were found to bind apoptotic cells. This study was limited by its retrospective nature, one consequence of which was lack of post-transplant patient serum samples.
Click to read the study in American Journal of Transplantation
Relevant Reading: Non-HLA transplantation immunity revealed by lymphocytotoxic antibodies
In-Depth [retrospective cohort]: This study examined pretransplant serum samples of 300 kidney transplant patients for IRAC as a predictive marker of transplant rejection. With a mean follow-up time of approximately 80 months, 46 of the 300 transplant patients experienced eventual transplant rejection. Thirty-seven percent of these graft rejections were a result of AMR. IgG antibodies purified from pretransplant patients and healthy specimen (n = 20) serum samples were evaluated for their reactivity to apoptotic Jurkat cells by flow cytometry. Mann-Whitney tests were used to compare reactivity of IgG between patient subgroups and between patients and healthy subjects. The Kaplan-Meier method was used to estimate survival events and comparisons were made using the log-rank test. Cox multivariate analysis accounted for confounding factors including reactivity to HLA antibodies, age, and race.
This study found that IRAC was significantly higher in kidney transplant candidates than in healthy subjects (p = 0.011) and was predictive of poor graft survival in transplant patients (hazard ratio = 2.271; p <0.001). Of the 46 failed graft patients, the 17 that experienced antibody-mediated rejection had significantly higher IRAC levels (p = 0.033). Particular subsets IgG1 and IgG3 were found to be most reactive to apoptotic cells.
More from this author: Modulating lymphocyte populations decreases graft rejection in mice,Adding Evolocumab to statin therapy further decreases LDL-C levels,Genetic variant linked to poor patient survival following lung transplantation, Genetic variations may predict outcomes for colorectal cancer patients, Neuroendocrine tumor marker pancreastatin may be predictive of survival
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.