Asciminib demonstrates superior efficacy for the treatment of CML in comparison to imatinib and second-generation TKIs
1. Asciminib demonstrated higher efficacy for the treatment of newly diagnosed CML than imatinib and second-generation TKI
2. Asciminib had a favorable safety profile compared to imatinib and second-generation TKIs.
Evidence Rating Level: 1 (Excellent)
Study Rundown: The present study is a phase three randomized controlled trial that set out to assess the efficacy of asciminib (a more specific TKI for the ABL myristoyl pocket) in comparison to an investigator-selected tyrosine kinase inhibitor (TKI) in the treatment of newly diagnosed CML. The primary outcome of the study was the major molecular response (MMR), defined as BCR::ABL1 transcript levels ≤0.1%, at week 48. Overall, the trial noted that asciminib demonstrated higher rates of major molecular response at 48 weeks compared to other TKIs, including imatinib. Further, asciminib demonstrated a favourable safety profile with fewer severe adverse events and less treatment discontinuation due to adverse events than other TKIs. Strengths of this trial include the comparison to multiple TKI inhibitors, which showed relative efficacy and safety profiles of asciminib across different patient risk categories. Limitations of this trial included a relatively short follow-up time of 48 weeks, which limits insights into long-term efficacy and safety. Overall, these findings suggest that asciminib may be a superior first-line treatment option for patients with newly diagnosed CML, although further studies are required to understand its long-term benefit.
Click to read the study in NEJM
Relevant Reading: A phase 3, open-label, randomized study of asciminib, a STAMP inhibitor, vs bosutinib in CML after 2 or more prior TKIs
In-Depth [randomized controlled trial]: This was a phase three, randomized controlled trial that assessed the efficacy and safety of asciminib in comparison to investigator-selected TKIs in patients with newly diagnosed CML. Patients were randomly assigned to receive either asciminib or an investigator-selected TKI, including imatinib and second-generation TKIs. The primary outcome was the MMR at week 48 (BCR::ABL1 transcript levels ≤0.1%). The study overall demonstrated that 67.7% of patients receiving the asciminib group achieved MMR at week 48, compared to 49.0% receiving investigator-selected TKI (95% confidence interval [CI], 9.6 to 28.2; P<0.001). When comparing asciminib with imatinib, 69.3% of patients treated with asciminib achieved MMR compared to 40.2% treated with imatinib (95% CI, 16.9 to 42.2; P<0.001). The authors additionally found that asciminib had a favorable safety profile. Patients on asciminib had fewer severe adverse events and a lower rate of treatment discontinuation due to adverse events compared to imatinib and second-generation TKIs. Severe adverse events occurred in 38.0% of patients receiving asciminib, compared to 44.4% and 54.9% in the imatinib and second-generation TKI group, respectively. The rate of treatment discontinuation due to adverse events was 4.5% for asciminib, 11.1% for imatinib, and 9.8% for second-generation TKIs. These findings suggest that asciminib demonstrated higher efficacy and a superior safety profile compared to existing TKIs for the treatment of newly diagnosed CML.
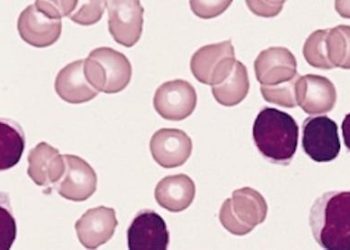
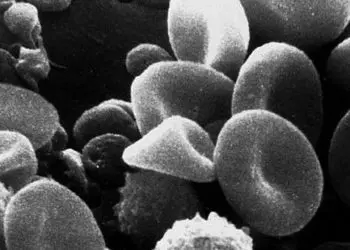
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.