Association of body mass index and extreme obesity with long-term outcomes following percutaneous coronary intervention
1. Patients with obesity undergoing percutaneous coronary intervention are typically younger with more cardiovascular risk factors, but may be less likely to experience procedural complications, short-term and long-term adverse outcomes, with the exception of patients considered extremely obese
Evidence Rating Level: 2 (Good)
It has been well established that obesity is associated with numerous adverse health outcomes and an increased risk of mortality. Interestingly, an “obesity paradox” has been described, where being obese or overweight may confer a protective effect for certain medical conditions when compared to patients with a normal body mass index (BMI). This may also be the case in the setting of percutaneous coronary intervention (PCI). In this cohort study, 25,413 patients that underwent PCI (January 2005-June 2017) were followed up for a median time of 4.4 years to evaluate the association between obesity and long-term survival after PCI. Of the patients comprising the cohort, 24.8% had a normal BMI while 3.3% were considered extremely obese (BMI ≥40). Researchers noted that with increasing BMI, patients were younger and exhibited more cardiovascular risk factors, including diabetes (p<0.001). Interestingly, however, with increasing BMI, the proportion of patients that presented non-ST-elevation acute coronary syndromes increased, whereas the proportion of patients presenting with ST-elevation myocardial infarction, out-of-hospital cardiac arrest, and cardiogenic shock decreased (p<0.001). With respect to PCI, there were no significant differences in the extent of coronary artery disease or lesion complexity between BMI groups, although drug-eluting stents were used more frequently in higher BMI patients (p<0.001). In addition, although overall infrequent, procedural complications were less common in higher BMI groups (p<0.04). In terms of clinical outcomes, specifically in-hospital and 30-day mortality, researchers observed a J-shaped association, where there was a steady decrease in mortality from the normal BMI group to the moderate obesity group, followed by a significant rise in mortality in the extreme obesity group (p<0.001). Similar relationships were noted between BMI and the incidence of major adverse cardiovascular events. Beyond 30 days, patients with moderate obesity had the lowest mortality rate at 12.2%, while patients with normal BMI or extreme obesity exhibited higher mortality rates at 19.2% and 14.1%, respectively. This study therefore shows that a moderately elevated BMI may be associated with reduced long-term mortality after PCI.
Click to read the study in Journal of the American Heart Association
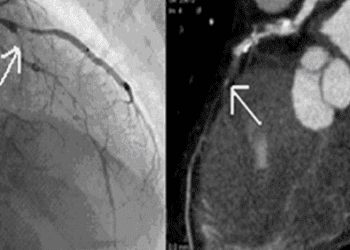
Image: PD
©2019 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.