Azithromycin use is associated with reduced maternal sepsis in vaginal deliveries
1. In this randomized controlled trial, a single dose of azithromycin reduced the risk of maternal sepsis or death among women in labor planning a vaginal birth as compared to a placebo.
2. Azithromycin use was not associated with a decreased risk of stillbirth, neonatal death, or neonatal sepsis.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Maternal infections are among the leading causes of maternal and neonatal mortality worldwide, disproportionately affecting individuals living in middle- and low-income countries. Azithromycin is a broad-spectrum antibiotic given, which is given intrapartum. It has been shown to be an effective form of prophylaxis during cesarian delivery to reduce maternal and neonatal infections. The current study was a randomized placebo-controlled trial aiming to investigate the effects of azithromycin on sepsis and mortality in pregnant women from low- or middle-income countries planning a vaginal delivery. Compared to a placebo, azithromycin resulted in a lower incidence of maternal sepsis or death but did not impact the rates of stillbirth, neonatal death, or neonatal sepsis. Azithromycin was not associated with an increased risk of adverse events. The trial was stopped prematurely during interim analysis due to maternal benefit. The study was limited by the low incidence of the primary outcomes in Asian countries and the lack of culture results of microorganisms from participants. Nevertheless, these results showed that in the setting of low-and middle-income countries, intrapartum azithromycin reduced the risk of maternal sepsis or death among women planning a vaginal birth.
Click here to read the study in NEJM
In-Depth [randomized controlled trial]: This study was a double-blinded, placebo-controlled, randomized trial conducted in seven low- or middle-income countries with high infant mortality rates. Pregnant women with singleton and multiple gestations of at least 28 weeks admitted to health facilities for a planned vaginal delivery were included. Exclusion criteria included advanced stage of labor infection warranting antibiotic use, arrhythmia, cardiomyopathy, allergy to or recent use of azithromycin, and planned cesarian delivery. In total, 29,278 women were randomized to receive a single two-gram prophylactic dose of azithromycin or placebo during labor. The primary outcomes were a composite of maternal sepsis or death by six weeks postpartum and a composite of stillbirth or neonatal death or sepsis by four weeks. The composite incidence of maternal sepsis or death was significantly lower in the azithromycin group (1.6%) than in the placebo group (2.4%) (Relative Risk [RR], 0.67; 95% Confidence Interval [CI], 0.56 to 0.79; p<0.001). However, the composite incidence of stillbirth or neonatal death or sepsis was comparable between the two groups (10.5% vs. 10.3%). The improvement in the maternal primary outcome was attributed to the lower incidence of maternal sepsis (1.5% [azithromycin] vs. 2.3% [placebo]; RR, 0.65; 95% CI, 0.55 to 0.77). The specific incidence rates of maternal death from any cause, neonatal sepsis, stillbirth, and neonatal death were comparable across both groups. During the interim analysis, the trial was stopped early due to maternal benefit observed in the azithromycin group. The incidence of adverse events was similar in the two groups, with none being significantly more prevalent with azithromycin use. In summary, these results suggested that among women planning a vaginal delivery, azithromycin could reduce the risk of maternal sepsis or death.
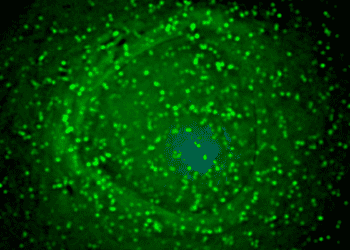
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.