Bapineuzumab does not improve clinical outcomes in Alzheimer’s disease
Image: PD
1. Bapineuzumab, a humanized anti-Aβ monoclonal antibody, did not improve clinical outcomes in patients with mild-to-moderate Alzheimer’s disease.
2. The most notable treatment-associated adverse events included neoplasm and amyloid-related imaging abnormalities with effusion or edema.
Evidence Rating Level: 1 (Excellent)
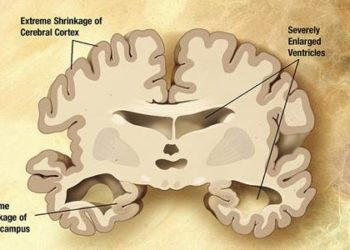
Study Rundown: Alzheimer’s disease is a significant challenge to affected patients and their caregivers, as well as the health care system at large. The amyloid hypothesis (see Relevant Reading) postulates that amyloid beta (Aβ) deposition in the brain parenchyma promotes further degenerative changes and may be a target for therapeutic intervention. The current study by Salloway et al. reports that bapineuzumab, a humanized anti-Aβ monoclonal antibody, did not improve cognition or functional ability in patients with mild-to-moderate Alzheimer’s disease. Separately, a trial involving solanezumab, a humanized anti-Aβ monoclonal antibody targeting a different region of the amyloid protein, has also failed to produce clinical improvement. This may be a temporary setback in the search for better therapeutic options, but also raises the possibility that therapies targeting Aβ alone may not adequately alter the course of neurodegeneration. The two trials reported in this study are both adequately powered, double-blind, placebo-controlled trials, each involving more than 1000 patients.
The study was funded by Janssen Alzheimer Immunotherapy and Pfizer.
Click to read the study in NEJM
Click to read an accompanying editorial in NEJM
Relevant Reading: The amyloid hypothesis of Alzheimer’s disease: progress and problems on the road to therapeutics
Study Author, Dr. Stephen Salloway, MD, MS, talks to 2 Minute Medicine: Director of Neurology and the Memory and Aging Program, Butler Hospital, Professor of Neurology and Psychiatry, Warren Alpert Medical School, Brown University
“With the aging of the population, the G-8 and the US Congress have made finding new treatments for Alzheimer’s disease by 2025 a top priority. These were the first large anti-amyloid monoclonal antibody trials. While the clinical outcomes were disappointing, we learned important new information that is already guiding new trials. This includes, treating AD earlier, when amyloid has a more critical role and brain injury is not well established, using amyloid biomarkers to focus treatment on those with amyloid pathology, combining treatments as we do in cancer, GOV, and heart disease to maximize benefit, and finding medications that can safely reduce amyloid burden to a greater extent.”
In-Depth [randomized controlled phase 3 trials]: This study is a composite of two trials – one involving apolipoprotein E (APOE) ε4 allele carriers and the other involving noncarriers. The primary outcome measures were scores on the 11-item cognitive subscale of the Alzheimer’s Disease Assessment Scale (ADAS-cog11) and the Disability Assessment for Dementia (DAD) at week 78. There were no significant differences observed between the bapineuzumab groups and the placebo groups in the carrier study or in the noncarrier study with respect to the primary outcomes. Additionally, there were no significant between-group differences in either study at week 78 on the following scores: Neuropsychological Test Battery, Clinical Dementia Rating-Sum of Boxes, MMSE, and the Dependence Scale.
Secondary outcome measures included findings on positron-emission tomographic amyloid imaging using Pittsburgh compound B (PIB-PET) and cerebrospinal fluid (CSF) phosphorylated tau (phospho-tau) concentrations. In the carrier study, the mean standardized uptake value ratio (SUVR), measured by PIB-PET, increased in the placebo group but remained almost unchanged in the bapineuzumab group. No significant increase in SUVR was observed in the placebo group in the noncarrier study. In the carrier study, a significant decrease in the CSF phospho-tau concentration was observed in the bapineuzumab group by week 71 (-5.80±1.49 pg/mL), compared to an increase in the placebo group (0.95±1.83 pg/mL). This represented a significant between group difference of -6.75 pg/mL (P=0.005). Among noncarriers, no significant between-group difference was observed (P=0.11).
In safety analyses, amyloid-related imaging abnormalities with effusion or edema were the most notable adverse events. This was detected in 15.3% of patients receiving bapineuzumab in the carrier study. Neoplasm was the most common fatal adverse event (6 cases [0.9%], all in the bapineuzumab group).
By Xiaozhou Liu and Adrienne Cheung
More from this author: Nivolumab plus ipilimumab shows promise for metastatic melanoma, Prophylactic platelet transfusions prevent bleeding in hematologic cancers, Azithromycin is not associated with increased cardiovascular death in low-risk groups, Health education module reduces parasitic infections, New chemotherapy precludes the need for radiotherapy in primary mediastinal B-cell lymphoma.
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.