Baricitinib protects β-cell function in new-onset type 1 diabetes
1. In this randomized controlled trial, the Janus kinase (JAK) inhibitor baricitinib was associated with preserved β-cell function compared to placebo in patients with new-onset type 1 diabetes mellitus (T1DM).
2. Patients receiving baricitinib also demonstrated tighter glycemic control compared to placebo.
Evidence Rating Level: 1 (Excellent)
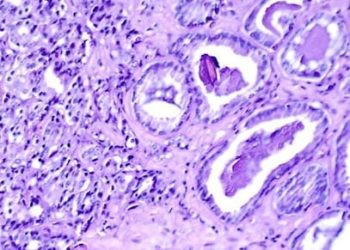
Study Rundown: The mainstay of T1DM treatment is exogenous insulin replacement due to a lack of disease-modifying therapies commonly employed in other autoimmune diseases. Insulin replacement, although life-saving, carries a high treatment burden and does not fully ameliorate the risk of diabetes-related complications. A key pathophysiological feature of T1DM is the JAK-mediated destruction of b-cells by CD8+ T cells. Baricitinib, a JAK1 and JAK2 inhibitor, has been shown pre-clinically to preserve b-cell function by blocking this pathway. This study was a randomized controlled trial to assess the efficacy and safety of baricitinib against a placebo in patients with new-onset T1DM. By 48 weeks, baricitinib was shown to result in higher levels of mixed-meal-stimulated C-peptide and reduced insulin requirement. Additionally, baricitinib recipients had lower variation in their glucose levels. Both groups had similar levels of glycated hemoglobin (HbA1c) by 48 weeks. Baricitinib was not associated with increased risks of adverse events compared to placebo. The study was limited by its small size and White-predominant demographics. Nevertheless, it was a first-of-its-kind study demonstrating baricitinib as a potential disease-modifying drug for T1DM.
Click here to read the study in NEJM
Relevant Reading: STAT1 Gain of Function, Type 1 Diabetes, and Reversal with JAK Inhibition
In-Depth [randomized controlled trial]: The current study was a randomized, placebo-controlled trial to evaluate baricitinib for patients with new-onset T1DM. Patients aged between 10 and 30 years who were diagnosed with T1DM within 100 days before starting baricitinib or placebo were eligible for inclusion. Exclusion criteria included treatment with other immunomodulatory drugs, co-existing cytopenias, cancer, history of thrombosis, or severe dyslipidemia. Overall, 91 patients were randomized 2:1 to receive either oral baricitinib 4mg once daily or placebo. The primary outcome was the median mixed-meal-stimulated C-peptide level at 48 weeks. Secondary outcomes included HbA1c change from baseline, daily insulin dose, and glycemic control as measured with continuous monitoring. By 48 weeks, the median mixed-meal-stimulated C-peptide level was 0.65 nmol/L/minute in the baricitinib group and 0.43 nmol/L/minute in the placebo group (p=0.001). Correspondingly, the mean daily insulin dose at this time was 0.41 U/kg/day (95% Confidence Interval [CI] 0.35 to 0.48) in the baricitinib group and 0.52 U/kg/day (95% CI 0.44 to 0.60) in the placebo group. The coefficient of variation in interstitial glucose measured continuously at 48 weeks was 29.6% (95% CI 27.8 to 31.3) in the baricitinib group and 33.8% (95% CI 31.5 to 36.2) in the placebo group. Notably, the mean HbA1c at 48 weeks was similar across both groups, 7.0% for baricitinib and 7.5% for placebo. The frequency and severity of adverse events were comparable between the two groups. These results showed that baricitinib was a potential disease-modifying drug that preserved β-cell function in new-onset T1DM.
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.