Buccal administration of dextrose gel effective for neonatal hypoglycemia
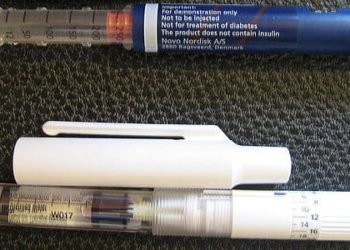
Image: CC/NICU
1. Administration of buccal dextrose gel to neonates is effective at correcting hypoglycemia within the first 48 hours of birth.
2. Buccal dextrose gel is easy to administer and allows for correction of neonatal hypoglycemia without separating mother and baby during treatment.
3. This is a cost-effective treatment ($2 per baby) that is well suited to treatments in resource-poor areas.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Hypoglycemia is an important cause of brain damage in the neonatal population. Up to 15% of otherwise healthy babies can be affected by the condition. Treatment is somewhat heterogeneous and varies dependent on the infant’s birth weight and gestational age. Often, initial management focuses on frequent blood glucose monitoring and feeding. If left uncorrected treatment escalates to possible NICU admission and administration of intravenous glucose. The authors of this study examined the use of buccal dextrose gel as a possible intervention given its effectiveness in the treatment of hypoglycemia in conditions such as adult diabetes and malaria in children. They found that buccal administration of 40% dextrose is effective at treating hypoglycemia in infants less than 48 hours old. Further, babies treated with dextrose gel group were more successful at breastfeeding, demonstrating decreased likelihood of receiving formula at two weeks of age as compared to controls. The strength of this study resides in the simple and inexpensive solution it proposes and tests. Indeed, avoidance of potential NICU admissions by administration of a $2 dextrose gel could have great value in preventing infant mortality and morbidity in a resource-poor setting. However, the study had some methodological flaws. More than half of the babies in the study were excluded from this analysis due to issues with the timing/placement of the interstitial glucose probe or measurement of the interstitial glucose concentration at the time of placement. A future study using a larger sample size and correcting for this methodological issue will be important to help provide a stronger argument in favor of the widespread implementation of dextrose gels for neonatal hypoglycemia.
Click to read the study, published today in The Lancet
Relevant Reading: Knowledge gaps and research needs for understanding and treating neonatal hypoglycemia
Study Author, Professor Jane E Harding, University of Auckland, New Zealand, talks to 2 Minute Medicine:
“Our study is the first report in babies showing that dextrose gel massaged into the inside of the cheek is more effective than feeding alone for treating hypoglycaemia, and is safe and simple to use.
Dextrose gel treatment costs roughly $2 per baby and could help reduce admissions to neonatal intensive care for treatment with intravenous glucose—not only reducing costs but importantly, keeping mothers and babies together to encourage breastfeeding”
In-Depth [randomized, double-blind, placebo controlled trial]: This study utilized 514 babies that were born at 35 weeks gestation or older and were less than 48 hours old. 242 of these babies became hypoglycemic, defined as a blood glucose less than 2.6 mmol/L and went on to receive buccal 40% dextrose gel or 2% carboxymethyl cellulose (placebo) gel. The babies underwent block randomization stratified by maternal diabetes status and birth weight to treatment vs. placebo groups. The primary study endpoint examined by the authors was treatment failure as defined as a blood glucose concentration less than 2.6 mmol/L 30 minutes after the second dose of gel. The results showed that administration of dextrose gel significantly decreased the frequency of treatment failure from 24% in the placebo group to 14% (RR 0.57, 95% CI 0.33-0.98; p=0.04). Secondary endpoints observed by the authors included NICU admission, breastfeeding frequency, total volume and frequency of expressed breast milk and formula, rebound and recurrent hypoglycemia after successful treatment, and total time with interstitial glucose levels less than 2.6 mmol/L. Importantly, buccal dextrose did not decrease the total all cause number of admissions to the NICU, but it did decrease the number of admissions solely due to hypoglycemia from 25% to 16% (RR 0.54, 95% CI 0.31 – 0.93; p=0.03).
By Devin Miller and Mimmie Kwong
More from this author: Racial backgrounds key to shaping the face of smoking-related mortality in South Africa, Probiotic formulations do not prevent antibiotic-associated diarrhea, Low statistical power leads to false reassurance when examining surgical outcomes, New surgical technique improves donor nerve localization in facial reanimation,A retrospective look at CPR use in surgical patients
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.