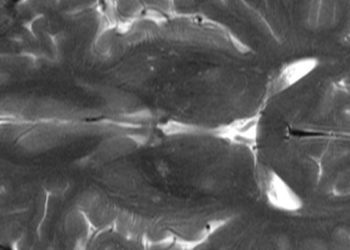
CAR-T Cell Therapy for Relapsed or Refractory High-Risk Neuroblastoma
1. GD2-CART01 infusion had an overall response of 63% of patients (33% complete response) with a 3-year overall survival of 60% in those who received the recommended dose.
2. No central neurotoxic effects were seen but 74% of patients had cytokine release syndrome (95% of those were mild).
Evidence Rating Level: 2 (Good)
Study Rundown: CAR T-cell therapy has been used in B-cell cancers, but there is less evidence in solid tumors. Neuroblastoma, a common solid tumor in children, expresses disialoganglioside GD2, which has been targeted with monoclonal antibodies to increase survival rates. This study was a phase 1-2 trial of GD2-CART01 in high-risk neuroblastoma patients. Phase 1 of the study showed no dose-limiting toxic effects and the recommended dose was 10×106 CAR-positive T cells/kg. Cytokine release syndrome occurred in 74% of patients after the first infusion of GD2-CART01 (largely grade 1 or 2) and no central neurotoxic effects were seen. With regards to longevity, GD2-CART01 cells were detected in vivo in 96% of patients and persisted for at least 3 months in 75% of evaluable patients. GD2-CART01 cells were found in bone marrow up to 2 years after infusion and in the cerebrospinal fluid in five patients up to 12 weeks after infusion. With regards to clinical response, complete response (CR) was 33%, partial response (PR) was 30%, 19% had stable disease, and 19% showed no response after 6 weeks post GD2-CART01 infusion. 3-year overall survival (OS) was 40% (60% if receiving full dose) and event-free survival (EFS) was 27% (36% if full dose). With a median follow-up of 1.7 years, 56% of patients with a CR had a maintained CR, with an OS of 66% and EFS of 50% at 3 years. The strengths of this study included the successful manufacturing of the GD2-CART01 and a long follow-up time. The limitations of the study included a small sample size and a single-arm approach. Overall, CAR-T cell therapy has the potential to cause long-lasting disease control in patients who have relapsed or refractory neuroblastoma.
Click to read the study in NEJM
Click to read an accompanying editorial in NEJM
Relevant Reading: Antitumor activity without on-target off-tumor toxicity of GD2-chimeric antigen receptor T cells in patients with neuroblastoma.
In-Depth [prospective cohort]: This was a phase 1-2 trial assessing the feasibility and safety of GD2-CART01 in 27 patients aged 1-25 with relapsed or refractory high-risk neuroblastoma. Phase 1 was designed as a dose-finding trial. All patients received fludarabine–cyclophosphamide lymphodepletion chemotherapy prior to infusion of GD2-CART01. Disease assessment was based on radiologic and MRI findings that were evaluated in a blinded fashion. GD2-CART01 manufacturing had a median viability of 90.5% (SD, ±3.7%) and a median transduction efficiency of 72.4% (SD, ±9.9%). In phase 1 of the study, there were no dose-limiting toxic effects reported and the recommended dose was 10×106 CAR-positive T cells/kg. Cytokine release syndrome occurred in 74% of patients after the first infusion of GD2-CART01 and was mostly grade 1 or 2 (one patient developed grade 3). Central neurotoxic effects did not develop in any of the patients. GD2-CART01 cells were detected in vivo in 96% of patients and persisted for at least 3 months in 75% of evaluable patients. GD2-CART01 cells were found in bone marrow up to 2 years after infusion and in the cerebrospinal fluid in five patients up to 12 weeks after infusion. The GD2-CART01 cells were also constructed with inducible caspase 9 (iC9) as a safety switch allowing the adoptively transferred cells to be killed if they were associated with dangerous toxic effects, and with patients receiving rimiducid (a dimerizing agent that induces caspase 9) a sharp decrease in the level of circulating GD2-CART01 was seen 4 hours after infusion of the dimerizing agent, but after 6 weeks, a new expansion of GD2-CART01, with levels that remained elevated at subsequent follow-up and were still detectable 30 months after infusion. With regards to clinical response, 33% of patients had a CR, 30% had a PR, 19% had stable disease, and 19% showed no response after 6 weeks post GD2-CART01 infusion. 3-year OS was 40% (60% if receiving full dose) and EFS was 27% (36% if full dose). With a median follow-up of 1.7 years, 56% of patients with a CR had a maintained CR, with an OS of 66% and EFS of 50% at 3 years. Those with a low disease burden had significantly longer survival than those with a higher disease burden, 3 years OS was 67% vs 0% (P<0.001). Overall, CAR-T cell therapy has the potential role in the treatment of refractory neuroblastoma.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.