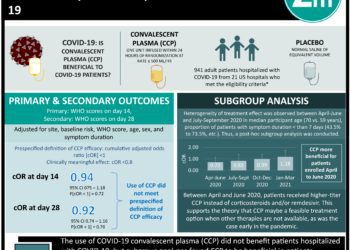
Convalescent plasma may not improve outcomes in Covid-19 patients
1. Convalescent plasma did not improve clinical outcomes in patients with severe pneumonia due to coronavirus disease 2019 (Covid-19) compared to placebo.
2. Convalescent plasma did not reduce 30-day mortality in patients with Covid-19 compared to placebo.
Evidence Rating Level: 1 (Excellent)
Study Rundown: The treatment of convalescent plasma is guided by the assumption of passive immunization jump starting the immune system in controlling disease evolution until a specific immune response is established. However, convalescent plasma treatment is only the standard of care for Argentine hemorrhagic fever. Furthermore, previous nonrandomized trials for the treatment of Middle East respiratory syndrome, influenza A (H1N1), and Ebola did not provide sufficient evidence for treatment effectiveness. With the known adequate safety profile of patients with coronavirus disease 2019 (Covid-19), this study evaluated the efficacy of convalescent plasma in the treatment of patients with Covid-19. The study determined convalescent plasma treatment did not significantly improve clinical outcomes or reduce 30-day mortality in patients with severe pneumonia due to Covid-19. The randomized control trial was limited by the study population. All of the patients had severe pneumonia, therefore, the effectiveness of the treatment could not be determined for patients with mild-to-moderate symptoms or life-threatening diseases. Nonetheless, this study’s results are significant, and its findings highlight the ineffectiveness of a treatment during an ongoing pandemic.
Click to read the study in NEJM
Relevant Reading: Safety update: COVID-19 convalescent plasma in 20,000 hospitalized patients
In-Depth [randomized controlled trial]: This randomized controlled trial enrolled 334 participants at 12 clinical sites in Argentina. Participants included in the study were ≥18 years of age, had a positive reverse-transcriptase-polymerase-chain reaction (RT-PCR) assay for the infection, and radiological confirmation of pneumonia. Participants who were pregnant or lactating, women of reproductive age unwilling to undergo contraceptive measures, and those with a history of blood component allergies were excluded from this study. The participants were randomized in a 2:1 ratio to receive convalescent plasma or placebo treatment, respectively. The primary outcome was clinical status 30 days after intervention. The participants were followed 30 days after intervention initiation. At the end of the follow-up period, there was no significant difference between the convalescent plasma group and the placebo group with regard to clinical outcome (odds ratio, 0.83; 95% confidence interval [CI], 0.52 to 1.35; P=0.46). Additionally, the 30-day mortality in the convalescent plasma group was 10.96% (25 of 228 participants) compared to 11.43% (12 of 105 participants) in the placebo group. The risk difference between both groups was -0.46 percentage points (95% CI, -7.8 to 6.8). The proportion of invasive ventilatory support requirements was 26.8% (61 of 228 participants) in the convalescent plasma group and 22.9% (24 of 105 participants) in the placebo group. Finally, infusion-related adverse events were more common in the convalescent plasma group (4.8%; 11 of 228 participants) than the placebo group (1.9%; 2 of 105 participants) (odds ratio, 2.62; 95% CI, 0.57 to 12.04). Taken together, convalescent plasma was not shown to improve clinical outcomes or reduce 30-day mortality in patients with severe pneumonia due to Covid-19.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.