Cost effectiveness of extending human papillomavirus vaccine administration until age 45
1. The FDA approved the expansion of the human papillomavirus (HPV) vaccination from ages 9 to 26 in women and 21 in men to 45 years in men and women.
2. This study predicted a small reduction in HPV-associated diseases and a substantially higher incremental cost-effectiveness ratios with extending the vaccination through age 45.
Evidence Rating Level: 3 (Average)
Study Rundown: The human papillomavirus vaccine has been recommended for females since 2006 and males since 2011 in the United States. The recommended age for vaccination was 11 to 12 years old up to age 26 for women and 21 years for men. In October 2018, the food and drug administration (FDA) expanded the age range to 9 years through 45 years old in males and females and was added to the U.S. Advisory Committee on Immunization Practices (ACIP) recommendations in August 2019. This study used mathematical modeling to estimate the effectiveness and cost-effectiveness of this added population that is approved to receive the HPV vaccine – women aged 27 to 45 years and men aged 22 to 45 years. The model predicted small reductions in HPV-associated disease including anogenital warts, CIN 2/3 cases, cervical cancer, and non-cervical HPV-associated cancer. In addition, vaccinating through age 45 is predicted to result in substantially higher incremental cost-effectiveness ratios (ICERs) than the current program.
Further research is required to examine herd effects of HPV vaccination, HPV infection burden after age 26, and identifying high risk populations that would benefit the most from adult vaccination.
Click to read the study in Annals of Internal Medicine
Relevant Reading: Systematic review of cost-effectiveness studies of human papillomavirus (HPV) vaccination: 9-Valent vaccine, gender-neutral and multiple age cohort vaccination
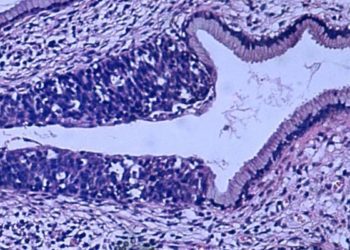
In-Depth [retrospective cohort]: This predictive analytic study used historical data on the effectiveness of the HPV vaccine in the United States to predict future outcomes with the new FDA age-expansion of the HPV vaccine to males and females through age 45. Four HPV vaccination scenarios were examined – vaccination of males and females up to ages 26, 30, 40, and 45 years. Vaccination uptake rates were kept concordant with historic rates, and efficacy was assumed at 2 doses for persons aged 9 to 17 and at 3 doses for adults. The main outcomes explored were the number of HPV-related outcomes avoided and cost per quality adjusted life year (QALY). Under the old HPV age recommendations, the vaccine is predicted to offer an 82% reduction in anogenital wart diagnosis, 80% reduction in cervical intraepithelial neoplasia (CIN) grade 2/3 cases, 59% reduction in cervical cancer cases, and 39% reduction in non-cervical HPV-associated cancer cases. With the age extension to 45 years old, the vaccine is predicted to reduce anogenital warts by an additional 0.4%, CIN 2/3 by 0.4%, cervical cancer by 0.2%, and non-cervical HPV-associated cancer by 0.2%. The additional cost per QALY gained is predicted to be $830,000 for vaccination through 30 years old, $1.843 million through 40 years old, and $1.471 million through 45 years old. The majority of model simulators produced ICERs greater than $124,000 for vaccination through 30 years old, $382,000 through 40 years old, and $463,000 through 45 years old per QALY gained.
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.