CYP2C19 loss-of-function carriers have modest benefit from ticagrelor and aspirin following cerebrovascular event: CHANCE-2 Trial
1. Patients carrying the CYP2C19 loss-of-function mutation (C-LOF), who had experienced a minor stroke or transient ischemic attack, experienced a significant reduction in risk of ischemic events within one week of starting ticagrelor/aspirin therapy.
2. Some minor additional benefit was accrued in the second week of dual therapy and was maintained in the following weeks.
Evidence Rating: 1 (Excellent)
Study Rundown: Patients who experience a cerebrovascular event (i.e., stroke or transient ischemic attack [TIA]) are at the greatest risk of subsequent stroke within the first three months of the incident event. Dual antiplatelet therapy (P2Y12 inhibitor medications, such as ticagrelor or clopidogrel, in combination with aspirin) is a well-established risk reduction strategy in the post-stroke period, although is associated with an increased risk of bleeding. Patients carrying a loss-of-function allele to the CYP2C19 gene are known to be less responsive to clopidogrel; therefore, the present study sought to determine the benefit of dual antiplatelet therapy with ticagrelor and aspirin in this population. 6412 patients were randomized in total, including 3205 in the ticagrelor group and 3207 in the clopidogrel group. The greatest reduction in risk of a cerebrovascular event for the CYP2C19 group was within the first week of initiating dual antiplatelet therapy. The beneficial effect of dual therapy was continuous, albeit less drastic in the subsequent weeks of the trial. Similarly, the increase in bleeding risk amongst the ticagrelor group was most notable in the first week of therapy, after which the risk remained relatively stable. The composite outcome of protection from stroke and moderate-severe bleeding favored the ticagrelor-aspirin group; this was consistent through the trial duration. The present trial by Pan et al demonstrated that patients with a CYP2C19 loss-of-function allele benefit from combined ticagrelor and aspirin therapy following a cerebrovascular event, and that the effect of therapy is most pronounced in the first week of treatment. This study contributes to an understanding of best practices in antiplatelet therapy post-stroke or TIA including choice of agent and duration of treatment. These findings are strengthened by the randomized trial design which does well to control for risk of bias. A primary limitation of this work is the stringent eligibility criteria which reduces the external validity of these conclusions.
Click here to read this study in JAMA Neurology
Click to read an accompanying editorial in JAMA Neurology
Relevant reading: Risk-benefit profile of long-term dual-versus single-antiplatelet therapy among patients with ischemic stroke: a systematic review and meta-analysis
In-Depth [randomized controlled trial]: A double-blinded, randomized controlled trial was conducted in more than 200 hospitals in China. Eligible patients were older than 40 years, carried the C-LOF allele, and had experienced an acute, non-embolic ischemic stroke or high-risk TIA. Patients who had received thrombolytic therapy or mechanical thrombectomy were excluded, as were patients who were currently taking anticoagulant(s). Patients were randomized in a 1:1 fashion to receive placebo, aspirin and ticagrelor, or placebo, aspirin and clopidogrel. The risk of cerebrovascular event after 1 week was 4.2% in the ticagrelor group and 5.7% in the clopidogrel group; the absolute risk reduction was 1.34% with a 95% confidence interval from 0.29-2.39%. The absolute risk reduction with 95% confidence intervals for the subsequent weeks of the trial was as follows: 0.11% (-0.24 to 0.45) in the second week, 0.14% (-0.11 to 0.38%) in the third week and 0.04% (-0.18 to 0.25) in the fourth week. The absolute increase in risk of bleeding in the ticagrelor/aspirin group was 0.87% (0.25 to 1.50) in the first week of the trial, 1.2% (0.75 to 1.68) in the second week, 0.33% (-0.05 to 0.72) in the third and 0.23% (-0.03 to 0.49) in the fourth week. These results were robust to sensitivity analyses, including weighting by intensity of bleeding events, or by intensity of initial cerebrovascular event.
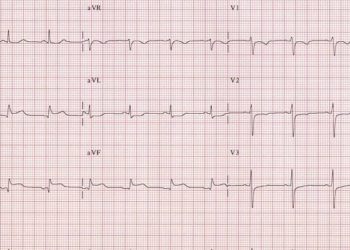
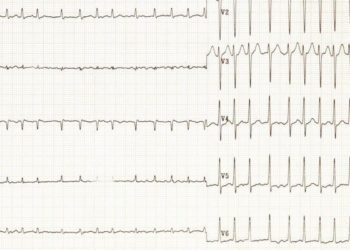
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.