Dietary patterns may have effects on outcomes of assisted reproductive technologies
1. For women with infertility on assisted reproductive technologies (ART), higher preconception adherence to dietary patterns for prevention of chronic disease were associated with lower probability of pregnancy loss, but no difference for clinical pregnancy or live birth.
Evidence Rating Level: 2 (Good)
The prevalence of infertility has been increasing over time, turning attention towards research into the use of assisted reproductive technologies (ART). Several studies have demonstrated associations between maternal dietary patterns and probability of pregnancy or live birth from using ART, including the Mediterranean diet. However, there have been inconsistent results due to disparities in how adherence to a diet is measured, and lack of comparison amongst different dietary patterns. Therefore, this current cohort study aimed to examine the correlation between 8 common dietary patterns and ART-related outcomes. The population included 612 women between 18 and 45 years of age, enrolled between 2007 and 2019, with 804 intrauterine insemination (IUI) cycles and 768 in-vitro fertilization (IVF) cycles. The women completed a validated questionnaire to evaluate their preconception diet’s adherence to the 8 dietary pattern, which included 3 Mediterranean diet indexes, the Healthy Eating Index (HEI) and Alternate Healthy Eating Index (AHEI), the American Heart Association (AHA) 2020 dietary goals Index, the DASH diet, and the plant-based diet (PBD). Outcomes evaluated included clinical pregnancy, live birth, clinical pregnancy loss, and total pregnancy loss (which included biochemical and clinical loss). The results showed no association between adherence to the 8 patterns and the outcomes of clinical pregnancy or live birth after either ART method. However, there was a lower risk of total and clinical pregnancy loss for women with higher adherence to the AHA dietary pattern: The probability of total pregnancy loss was 0.41 (95% CI 0.33-0.50) vs 0.28 (95% CI 0.21-0.36, p for trend = 0.02) for the lowest vs highest quartile adherence to the AHA diet, whereas the probability of clinical pregnancy loss was 0.30 (95% CI 0.22-0.39) vs 0.15 (95% CI 0.10-0.23, p for trend = 0.007) for the lowest vs highest quartiles. A similar but weaker association was found for other patterns, including the HEI, AHEI, and 3 Mediterranean diet scores, but not the PBD. Overall, this study demonstrated the association between higher preconception adherence to specific dietary patterns for prevention of chronic disease and lower probability of pregnancy loss on ART, but not clinical pregnancy or live birth.
Click to read the study in JAMA Network Open
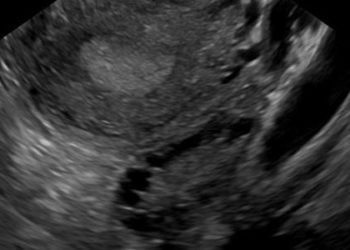
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.