Digestive tract decontamination associated with low antibiotic resistance in ICU
1. Selective decontamination of the digestive tract (SDD) was associated with a lower prevalence of antibiotic-resistant gram-negative bacteria in the rectum compared to selective oropharyngeal decontamination (SOD).
2. There were no differences in ICU lengths of stay or day-28 mortality between the two groups.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Prophylactic antibiotic regimens such as selective decontamination of the digestive tract (SDD) and selective oropharyngeal decontamination (SOD) in intensive care units (ICUs) have been shown to lower the incidence of respiratory infections. However, no studies have examined the patterns of antibiotic resistance in the ICU associated with their usage. The authors of this study conducted a cluster randomized crossover trial to administer SDD or SOD for 12 months in ICUs in order to study the prevalence of antibiotic-resistant gram-negative bacteria. The authors were also interested in day-28 mortality, ICU-acquired bacteremia, and ICU length of stay. Compared to SOD, SDD was associated with a lower prevalence of antibiotic-resistant gram-negative bacteria in the rectum and a lower rate of ICU-acquired bacteremia. There were no differences in ICU lengths of stay or mortality.
The major strengths of this study include its study design. It included over 5,000 patients in each group in a cluster randomized crossover trial. One limitation is that it did not include a control group in which ICUs administered neither SOD or SDD. However, previous studies showed that SOD or SDD decreased mortality and it was thus considered unethical to withhold both regimens. Additionally, a subset of ICUs used ceftriaxone instead of cefotaxime during SDD. However, the authors note that both antibiotics have similar microbial coverage and their differing usage may merely reflect variations in clinical practice. Overall, this study suggests that SOD may be favored over SDD in future clinical practice, since SDD is more expensive without any observed improved benefits in mortality.
Click to read the study, published today in JAMA
Click to read an accompanying editorial, published today in JAMA
Relevant Reading: Infection control measures to decrease the burden of antimicrobial resistance in the critical care setting
In-Depth [cluster randomized crossover trial]: Sixteen ICUs in the Netherlands were randomized to either SDD or SOD for 12 months followed by crossover to the other intervention for another 12 months. The primary outcome was unit-wide prevalence of antibiotic-resistant gram-negative bacteria. While SOD was associated with a higher prevalence of aminoglycoside resistant gram-negative bacteria compared to SDD (11.8% vs. 5.6%, p<0.001), the rectal carriage of this bacteria increased more with SDD than SOD (7% vs 4% per month, p=0.046). Secondary outcomes were day-28 mortality, ICU-acquired bacteremia, and ICU length of stay. There was no difference in day-28 mortality (adjusted OR 0.96; 95%CI 0.88-1.06) or length of stay in the ICU (HR 0.96; 95%CI 0.92-1.01) between the two groups. ICU-acquired bacteremia was lower in the SDD group compared to the SOD group (OR 0.77; 95%CI 0.65-0.91).
More from this author: Incidence and prevalence of diabetes in US stabilizing, Guided patient self-management of blood pressure medications effective, Flexible sigmoidoscopy decreases colorectal cancer incidence and mortality, Stroke within past 9 months linked with adverse surgical outcomes, Home initiation of HIV care increases anti-retroviral therapy use in Malawi, Immune-modulating enteral nutrition does not reduce infections in the ICU
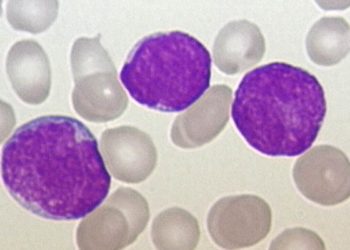
Image: PD
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.