Direct oral anticoagulants associated with lower risk of osteoporotic fracture versus warfarin
1. In this observational study, patients who received one of three direct oral anticoagulants (DOACs) were significantly less likely to have an osteoporotic hip or vertebral fracture compared to those who received warfarin.
2. No difference in fracture risk was detected between individual DOACs.
Evidence Rating Level: 2 (Good)
Study Rundown: Osteoporotic fracture has a very high morbidity and mortality, especially among older individuals. Warfarin is commonly used for stroke prevention, but its detrimental effects on vitamin-K dependent proteins involved in bone metabolism have led to speculation that its use may increase the risk for osteoporosis. A number of direct oral anticoagulants (DOACs) exert a prophylactic effect equal to that of warfarin, are associated with a lower bleeding risk, and require less monitoring, making them promising as treatment alternatives. However, since patients who require anticoagulant management are also often predisposed to osteoporosis, it is important to investigate the role of these agents in fracture risk. This observational study found that, in patients with atrial fibrillation, those who received DOACs had a significantly lower risk for osteoporotic fractures compared to those who received warfarin, but no difference was detected between the individual DOACs. While women had a higher overall incidence of fracture than men, these associations were observed in both sexes, and they suggest an additional advantage of DOACs over warfarin. A limitation of the study was the failure to account for potential confounding variables such as body mass index and bone mineral density, but these factors were unlikely to have caused significant differences in anticoagulant prescribing.
Click here to read the study, publish today in Annals of Internal Medicine
Relevant Reading: Anticoagulants and Osteoporosis
In-Depth [prospective cohort]: This Hong Kong territory-wide study included data from 23,515 adults who were diagnosed with atrial fibrillation between 2010 and 2017 and started on 1 of 4 anticoagulants: apixaban (3241 patients), rivaroxaban (3866 patients), dabigatran (6867 patients), or warfarin (9541 patients). The mean age of included participants was 74.4 years (standard deviation, 10.8), and all baseline characteristics (age, sex, index year, comorbidities, history of falls/fractures, medication use, etc.) had standardized differences below 0.15 after propensity-score weighting. A total of 401 hip or vertebral fractures were reported, with 49% occurring in the warfarin group alone. At 24 months, the adjusted cumulative incidence differences (CIDs) from warfarin were -0.88% (95% confidence interval [CI], -1.66% to -0.21%) for apixaban, -0.81% (95% CI, -1.34% to -0.23%) for dabigatran, and -1.13% (95% CI, -1.67% to -0.53%) for rivaroxaban. These corresponded to hazard ratios of 0.62 (95% CI, 0.41 to 0.94) for apixaban, 0.65 (95% CI, 0.49 to 0.86) for dabigatran, and 0.52 (95% CI, 0.37 to 0.73) for rivaroxaban. The CIDs between DOACs ranged from -0.06% to -0.32% but were not statistically significant.
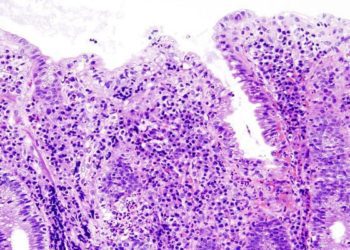
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.