Drug-eluting scaffold superior to angioplasty for infrapopliteal artery disease
1. In this randomized controlled trial, for patients with chronic limb-threatening ischemia (CLTI) due to infrapopliteal artery disease (IAD), a drug-eluting resorbable scaffold was superior to angioplasty in reducing the risk of vascular events.
2. There was no significant difference in the adverse events between the drug-eluting resorbable scaffold and angioplasty groups.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Peripheral artery disease is an epidemic, and its incidence is increasing alongside other cardiovascular diseases. The most severe complication is CLTI, and affected patients are at high risk of amputation and death. For those with CLTI due to IAD, angioplasty demonstrated superiority to open procedures, but it is associated with limited durability. Drug-eluting resorbable scaffolds offer the advantage of mechanical support, delivery of antiproliferative agents, and resorption allowing for favorable vessel remodeling and future intervention. This study compared everolimus-eluting resorbable scaffold against angioplasty for CLTI due to IAD. At one year, the composite risk of amputation, vessel occlusion, revascularization, or restenosis was significantly lower among the scaffold group than the angioplasty group. The rates of adverse events, including major adverse limb events and perioperative death, were comparable between the two groups and demonstrated noninferiority. The study was limited by a small and specific patient sample, and the scaffold was only employed in the proximal two-thirds of the infrapopliteal arteries. Nevertheless, it supported that an everolimus-eluting resorbable scaffold was superior to conventional angioplasty in treating CLTI secondary to IAD.
Click here to read the study in NEJM
In-Depth [randomized controlled trial]: The current study was a randomized controlled trial comparing everolimus-eluting resorbable scaffold against angioplasty in treating CLT due to IAD. Patients 18 years of age or older presenting with CLTI due to IAD, with specific anatomical criteria such as the lesions located within the proximal two-thirds of the infrapopliteal arteries and the lengths of scaffold required to treat less than 170mm, were included. Exclusion criteria included severe lesions and those outside anatomical criteria, pregnancy, recent amputation, serious kidney disease, recent stroke, and immunosuppressive diseases. Two hundred sixty-one patients were randomized 2:1 to receive an everolimus-eluting resorbable scaffold or angioplasty. The primary efficacy outcome was freedom from amputation above the ankle of the target limb, complete occlusion of the target vessel, need for revascularization, and binary restenosis of the target lesion at one year. The primary safety outcome was freedom from major adverse limb events at six months and perioperative death. Overall, the primary efficacy outcome occurred in 74% of patients in the scaffold group and 44% of the angioplasty group (absolute difference 30 percentage points; 95% Confidence Interval [CI], 15 to 46; p<0.001 for superiority). Binary restenosis occurred in 24% of patients in the scaffold group and 50% of the angioplasty group (p<0.001 for superiority). The primary safety outcome was observed in 97% of the scaffold group and 100% of the angioplasty group (absolute difference -3 percentage points; 95% CI -6 to 0; p<0.001 for noninferiority). In summary, these results demonstrated the potential advantage of drug-eluting resorbable scaffolds over angioplasty in treating CLTI due to IAD.
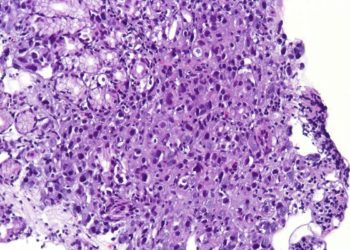
Image: PD
©2024 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.