Early and delayed renal-replacement therapy for septic shock associated acute kidney injury show similar mortality: the IDEAL-ICU trial
1. Among patients with septic shock and acute kidney injury (AKI), there was no significant difference in 90-day mortality between early (within 12 hours) and delayed (after 48 hours) initiation of renal-replacement therapy (RRT).
2. Patients in the delayed group had significantly more days free from RRT, with no significant differences compared to the early group in mechanical ventilation or vasopressor requirements, or duration of intensive care unit (ICU) or hospital length of stay.
Evidence Rating Level: 1 (Excellent)
Study Rundown: AKI is a common and life-threatening complication of septic shock. While RRT is the cornerstone of management, there is controversy over the initiation and appropriate timing in the absence of emergent indications. This trial aimed to determine whether there was a mortality difference between the initiation of RRT within 12 hours after the diagnosis of failure-stage AKI due to septic shock or after a delay of 48 hours. The primary outcome, overall mortality at 90 days, demonstrated no significant difference between early and late initiation of RRT. The patients in the delayed initiation arm were exposed to significant less days of RRT; however, there were no significant differences among any other key secondary outcomes, including: mortality at 28 days and 180 days, number of days free from mechanical ventilation or vasopressors, length of ICU stay, or length of hospital stay. The results of this trial suggest that early initiation of RRT may unnecessarily expose patients with septic shock and AKI to the risks of this therapy in whom renal function may spontaneously recover, without any mortality benefit.
This multicenter, randomized trial was based on large sample size and provides high-quality evidence on the issue of RRT timing in AKI from septic shock, a subject which previous trials have shown discordant results. The study was limited by the use of the RIFLE (Risk, Injury, Failure, Loss of kidney function, and End-stage kidney disease) classification to document AKI, which may not be generalizable to patients with AKI based on different criteria. Furthermore, 48 hours may not be sufficient for some patients to spontaneously recover renal function.
Click to read the study in NEJM
Relevant Reading: Initiation strategies for renal-replacement therapy in the intensive care unit
In-Depth [randomized controlled trial]: This was a multicenter trial conducted across 29 ICUs in France that randomized 488 patients with septic shock and documented AKI to an early-strategy (within 12 hours of AKI diagnosis, n=246) or delayed-strategy (after 48 hours of AKI diagnosis, n=242) of RRT initiation. AKI was diagnosed if one criterion in the failure stage of the RIFLE classification was met. Immediate RRT was initiated in the delayed-strategy group if any of the established criteria for emergency RRT were met, and was not initiated in patients if spontaneous renal recovery occurred. RRT modality was based on physician discretion. The primary outcome was death from any cause at 90 days after randomization. Key secondary outcomes included the number of days free from RRT, mortality at 28 days and at 180 days, use of mechanical ventilation and vasopressors at 28 days, and length of ICU or hospital stay.
Among the 477 patients (early strategy, n=239; delayed-strategy, n=238) in whom follow-up data was available, there was no difference in 90-day mortality (58% in the early-strategy group and 54% in the delayed-strategy group; P=0.38). The delayed-strategy demonstrated a significantly larger number of days free from RRT than the early-strategy (median days, 16 vs. 12, respectively; P=0.006). A total of 70 patients in the delayed-strategy group spontaneously recovered renal function and therefore did not receive RRT. There was no significant difference between the treatment groups in any other secondary outcome, including: mortality at 28 days, mortality at 180 days, median days free from mechanical ventilation, median days free from vasopressors, median length of ICU stay, or median length of hospital stay.
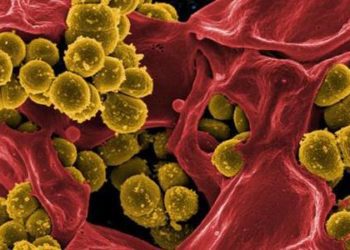
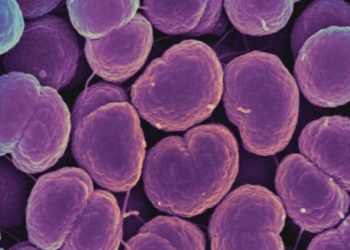
Image: PD
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.