Electronic health records associated with significant improvement in diabetes mellitus control measures
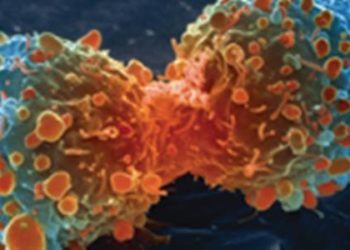
Image: CC/Jodi
Key Findings:
- Implementing electronic health records in 17 centres was associated with significantly improved HbA1c and LDL-C control in patients with diabetes mellitus
- Electronic records were also linked with more guideline-concordant practice, including more appropriate treatment intensification and follow-up testing
Primer: Electronic health records are often considered integral to advancing the practice of medicine and improving the quality of health care. Proponents of electronic health records argue that they reduce the likelihood of medical errors, improve efficiency by avoiding redundancy in testing, and increase accessibility to health information. While the theoretical benefits are certainly intriguing, actual experiences with electronic records have yielded mixed results with regards to improving health care delivery. And while many large scale initiatives are being undertaken to encourage health care providers to adopt electronic health records, there is little evidence exploring their effects on clinical outcomes, particularly in managing chronic diseases. Published recently in the Annals of Internal Medicine, this study sought to explore the effects of implementing electronic health records on clinical care pathways and outcomes for patients with diabetes mellitus.
For further reading, please see the following studies:
- Buntin MB, Burke MF, Hoaglin MC, et al. The benefits of health information technology: A review of the recent literature shows predominantly positive results. Health Affairs 2011;30:464-471.
- Chaudhry B, Wang J, Wu S, et al. Systematic review: Impact of health information technology on quality, efficiency, and costs of medical care. Ann Intern Med 2006;144:742-752.
The [observational, quasi-experimental] study: A quasi-experimental study was conducted looking at measures of diabetes mellitus control before and after the implementation of electronic health records at 17 different centres. Measures of control were glycated hemoglobin (HbA1c) and low-density lipoprotein cholesterol (LDL-C) levels. A total of 169,711 patients were included in the final analysis. The study demonstrated a significant increase in treatment intensification for patients with HbA1c ≥7% and in the probability of follow-up testing within one year after the implementation of electronic health records. Moreover, electronic records were associated with a significant decrease in retesting for individuals with good control. Significant reductions in HbA1c and LDL-C were achieved with the implementation of electronic records.
In sum: The adoption of electronic health records at 17 centres resulted in significant improvements in appropriate treatment intensification, follow-up testing, and HbA1c and LDL-C measures in patients with diabetes mellitus. Moreover, for individuals with sufficient control, there was a significant reduction in repeated testing. These findings suggest that electronic health records encourage more guideline-concordant diabetes management.
Limitations of this study include questions regarding generalizability, as electronic health records are often impacted by numerous contextual factors, and the observational study design. Given that electronic health records are being rapidly impelemented in many jurisdictions, this study adds to the body of evidence justifying its use in managing chronic diseases.
Click here to read study in Annals of Internal Medicine
Written by [AdC] and [AC]
© 2012 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. DISCLAIMER: Posts are not medical advice and are not intended as such. Please see a healthcare professional if you seek medical advice.