Entinostat plus azacitidine may not improve response for myelodysplastic syndrome
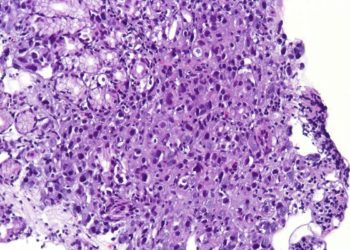
Image: PD
1. Adding entinostat to azacitidine (AZA) therapy for myelodysplastic syndrome (MDS) or acute myeloid leukemia (AML) with myelodysplasia-related changes does not improve rates of hematologic normalization (HN).
2. Increased duration of AZA therapy increases HN rate compared to standard dosing.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Previous trials have demonstrated improved survival in high-risk MDS with azacitidine (AZA) therapy, and so AZA has become the standard of care for these patients. However, 40-50% of patients do not respond. The purpose of this phase II trial was to evaluate whether adding entinostat to AZA therapy improves the treatment response rate. Upon analysis, the authors found that HN did not significantly differ between the two treatment arms, suggesting that entinostat does not improve treatment response to AZA. They also found that there was an improved response to a longer, lower-dose AZA regimen as compared to previous trials. Based on these results, the authors concluded that while entinostat did not demonstrate any improvement in response, further investigation into the optimal dosing schedule for AZA with a focus on overall survival is warranted. It should be noted that, while the randomized, controlled design of this study supports its results, that the participation of AML patients may limit comparisons with previous trials of AZA efficacy.
Click to read the study in JCO
Relevant Reading: Randomized controlled trial of azacitidine in patients with the myelodysplstic syndrome: a study of the cancer and leukemia group B
In-Depth [randomized controlled trial]: In order to evaluate the impact of additional entinostat therapy, the authors designed a phase II controlled trial enrolling a total of 150 patients. To be included, patients were diagnosed with MDS, chronic myelomonocytic leukemia or AML-MRC. Patients who had been previously treated with entinostat, stem cell transplant or induction chemotherapy were excluded. They were then randomized to either AZA alone (given for 10 days rather than the FDA 7 day schedule) or to AZA as well as entinostat. The primary outcome measured was the rate of hematologic normalization, defined as achieving complete or partial remission or trilineage hematological improvement. HN was 32% in the AZA only group (95% CI, 22% to 44%) and 27% in the combined therapy group (95% CI, 17% to 39%). With a follow-up time of 30 months, overall survival was 18 months in the first arm and 13 months in the second arm.
More from this author: Rituximab linked with reduced chronic immune disease following stem cell transplantation, High-dose prophylaxis for hemophilia increases costs with minimal benefit, Ambrisentan found ineffective against idiopathic pulmonary fibrosis
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.