Enzalutamide reduces risk of metastatic prostate cancer in at-risk men
1. Prostate cancer patients with a rapidly risking prostate-specific antigen (PSA) despite chemical or physical castration had lower rates of metastasis when treated with enzalutamide compared to those in a placebo group.
2. No difference in overall survival was observed between the treatment and placebo groups at a median follow-up time of 18.4 and 11.1 months for the two groups, respectively.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Prostate cancer is associated with metastasis, and rapidly rising PSA and castration-resistant subtypes of prostate cancer are significant metastatic risk factors. For men considered at-risk for metastasis hormonal therapy is used to prolong metastasis-free (MFS) and overall (OS) survival, though clinical evidence supporting some of these methods are limited. Enzalutamide binds to the androgen receptor and inhibits downstream androgen effects. Previous work has shown enzalutamide treatment can increase both progression-free (PFS) and OS. The PROSPER trial sought to assess effect of enzalutamide on MFS in patients with castration-resistance and rapidly rising PSA. Median MFS was significantly greater in patients treated with enzalutamide compared to placebo, and time until subsequent antineoplastic therapy was also significantly longer in the treatment group.
Strengths of this study include thorough reporting of adverse outcomes and international, multi-institutional design. Limitations include lack of reporting on treatments the patients may have undergone, including radiation and/or surgeries.
Click to read the study, published in NEJM
Relevant Reading: The evolutionary history of lethal metastatic prostate cancer
In-Depth [randomized controlled trial]: This double-blind, phase 3 randomized controlled trial enrolled patients between 2013 and 2017. Eligible patients had prostate adenocarcinoma with rising PSA (doubling time of less than 10 months) despite testosterone levels consistent with castration as all patients either had a bilateral orchiectomy or had been receiving androgen deprivation therapy. Patients had no metastatic disease as confirmed by CT or MRI, and whole-body radionuclide scanning. Patients were randomized into enzalutamide (n = 933) and placebo (n = 468) groups. Evaluation for metastasis by radiographic imaging was performed every 16 weeks during follow-up. The primary endpoint was MFS starting from randomization and key secondary endpoints included PSA progression and OS.
At a median duration of trial follow-up of 18.4 months in the treatment group and 11.1 months in the placebo group, median MFS was 36.6 months in the treatment group and 14.7 months in the placebo group. Enzalutamide was associated with a 71% lower risk of metastasis than placebo (hazard ratio [HR], 0.29; 95% confidence interval [CI], 0.24 to 0.35; p < 0.001). PSA progression occurred in 69% of the placebo group and 22% of the control group (p < 0.001). There was no significant difference in overall survival between the treatment (11%) and placebo (13%) groups (p = 0.15). Enzalutamide treated patients used subsequent antineoplastic therapy at a lower rate than placebo patients (15% vs 48%, p < 0.001).
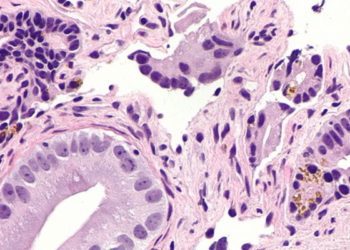
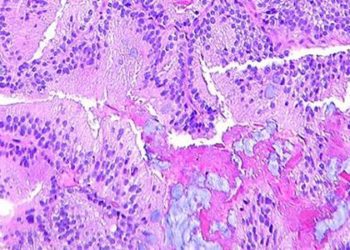
Image: CC/Wiki
©2018 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![2 Minute Medicine: Pharma Roundup: Price Hikes, Breakthrough Approvals, Legal Showdowns, Biotech Expansion, and Europe’s Pricing Debate [May 12nd, 2025]](https://www.2minutemedicine.com/wp-content/uploads/2025/05/ChatGPT-Image-May-12-2025-at-10_22_23-AM-350x250.png)