False-positive screening mammography results associated with increased risk of breast cancer
1. As compared to patients with negative mammograms, women with false-positive results on mammography displayed an increased risk of breast cancer, which was significantly higher among patients with calcifications present on mammography.
2. Breast cancer risk was further increased among women with multiple false-positive mammograms over time, particularly for those in which abnormal mammographic findings changed over time.
Evidence Rating Level: 2 (Good)
Study Rundown: Routine mammographic screening for breast cancer is recommended for women between 40 and 75 years of age to improve the probability of early stage detection and treatment. Despite the value of screening remains an imperfect tool; false positives results are not uncommon and subject patients to the emotional, physical and financial burden associated with follow-up testing. False-positive results are however based on abnormal findings on screening mammograms, and may represent the presence of benign breast disease or even preneoplastic changes that are not appropriately sampled during follow-up testing. The present retrospectively examined a large cohort of women from the Spanish Breast Cancer Screening Program who underwent mammographic screening, following those with subsequent false-positive results for interval development of breast cancer. As compared to women with true-negative results, women with false-positive results at mammography were at a significantly increased risk of later breast cancer development, particularly among women with radiographic evidence of calcifications, or with two or more false-positive results. The data from this study further suggested that the risk of breast cancer among women with prior false-positive screening mammograms was similar between both interval cancers and those detected at subsequent screening. Taken together, knowledge of the increased risk of false-positive screening results may and features such as calcifications may be helpful in developing improved risk-prediction models and follow-up imaging protocols within this particular population. Strengths of this study include its lengthy follow-up period and large sample size, which strengthens the power of its findings, however the study was limited in that investigators were unable to confirm for all involved patients if the subsequently detected tumors were found at the same location as the initially noted false-positive features on mammography.
Click to read the study in Radiology
Relevant Reading: Reduction in false-positive results after introduction of digital mammography: analysis from four population-based breast cancer screening programs in Spain
In-Depth [retrospective cohort]: Researchers reviewed medical records of 521 200 women between the ages of 50 and 69 who underwent screening mammography as part of the Spanish Breast Cancer Screening Program between 1994 and 2010, with a follow-up interval until December 2012. The age-adjusted hazard ratios (HR) of disease development were estimated using Cox proportional hazards regression analysis. Accounting for both subsequent screen-detected and interval cancers, and for screen-film and digital mammography, the age-adjusted HR of cancer in women with false-positive results was 1.84 as compared to women with negative mammograms (95% CI: 1.73, 1.95; p < 0.001). The risk was higher in women who had calcifications, whether they were (HR: 2.73; 95% CI: 2.28, 3.28; p < 0.001) or were not (HR: 2.24; 95% CI: 2.02, 2.48; P < 0.001) associated with masses. Women in whom mammographic features showed changes in subsequent false-positive results were those who had the highest risk (HR: 9.13; 95% CI: 8.28, 10.07; p < 0.001). The risk of breast cancer in women with false-positive results was similar between screen-detected (HR: 1.77; 95% CI: 1.65, 1.90) and interval (HR: 2.01; 95% CI: 1.81, 2.24) cancers.
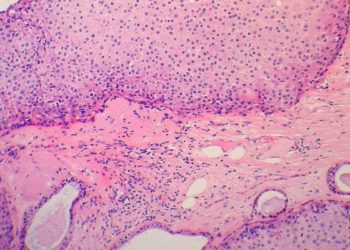
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.