Fecal occult-blood testing linked with reduction in colorectal-cancer mortality
Image: PD
1. Across a 30-year follow-up period, annual and biennial fecal occult-blood testing groups had a risk of death from colorectal cancer that was 32% and 22% lower, respectively, than that of unscreened controls.
2. There was no reduction in all-cause mortality between the combined screening groups and the control group.
Evidence Rating Level: 1 (Excellent)
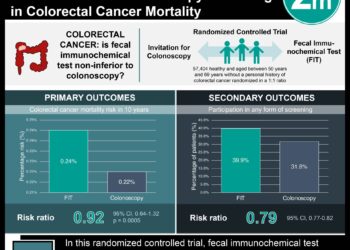
Study Rundown: In this randomized control study, the authors followed a large cohort of healthy volunteers across a 30-year follow-up period and showed that the annual and biennial fecal occult-blood testing (FOBT) groups had a risk of death from colorectal cancer that was 32% and 22% lower, respectively, than that of unscreened controls. Men between 60 to 69 years of age benefited the most, while no significant benefits of screening were found among women less than 60 years of age. Despite the large sample size, the authors did not observe any reduction or trend toward a reduction in all-cause mortality between the screening groups and the control group.
This study provides grounding for the continued use of fecal occult-blood testing along with colonoscopy for colorectal-cancer screening, in keeping with current colorectal-cancer screening guidelines. Randomized trials are ongoing to compare directly between FOBT and colonoscopy, but prior research has shown that FOBT offered in conjunction with colonoscopy can increase rates of colorectal-cancer screening. Furthermore, advances in FOBT technology, including the fecal immunochemical test (FIT) have made this a more desirable screening platform. Strengths of this study include the large sample size and the observation of a colorectal-cancer mortality reduction that was consistent across a 30-year study period. This latter finding was suggestive of the effect of removing adenomas presumably found after FOBT screening that would have progressed to cancer and death.
A notable drawback of the study was that information on vital status and cause of death was collected from death certificates, with a substantial interval between time of death and availability of the information. Further, there were no data regarding the screening history of trial participants after the original trial ended, so the result measures include the effect of unknown screening behaviors in the interim period.
Click to read the study, published today in NEJM
Click to read an accompanying editorial in NEJM
Relevant Reading: Should we use total mortality rather than cancer specific mortality to judge cancer screening programmes?
In-Depth [randomized, controlled trial]: This study randomized 46,551 healthy volunteers, aged 50 to 80 years, to three groups: annual or biennial screening with FOBT, or usual care (control). The primary end point was colorectal-cancer mortality. Screening took place between 1976 and 1992, with a 4-year hiatus from 1982 to 1986. Individuals found to have a positive FOBT underwent typical diagnostic workup including colonoscopy with polypectomy if necessary (complication incidence 0.1%). 90% of participants completed at least one FOBT, and the follow-up rate for positive tests was 83%. In 2011, mortality end points after 30 years of follow-up were assigned through a National Death Index database search in order to determine the cause of death as colorectal-cancer related or other.
After 30 years of follow-up, there were 33,020 deaths in total. Those specifically attributed to colorectal cancer were 1.8%, 2.2%, and 2.7% of deaths in the annual-screening, biennial-screening, and control groups respectively. The relative risk of death from colorectal cancer was 0.68 (95% CI, 0.56 to 0.82) with annual screening and 0.78 (95% CI, 0.65-0.93) with biennial screening. Annual or biennial screening with FOBT did not have a significant effect on all-cause mortality; the relative risk of death from any cause was 1.00 (95% CI, 0.99 to 1.01) with annual screening and 0.99 (95% CI, 0.98 to 1.01) with biennial screening. In subgroup analysis, the reduction in colorectal-cancer mortality was larger for men than for women in both screening groups. The interaction between sex and screening, measured by the ratio of the relative risk for men to that of women, was significant in the biennial screening group (P=0.04 for interaction). There was no benefit to screening among women less than 60 years of age.
By Matthew Growdon and Adrienne Cheung
More from this author: Alternative treatment for acute promyelocytic leukemia promising, The CHEST-1 & PATENT-1: Riociguat significantly improves exercise capacity in pulmonary hypertension patients, High glucose levels associated with increased risk of dementia, Insecticidal bed nets linked with reduced transmission of lymphatic filariasis
© 2013 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.