Fluoroscopically-guided lumbar punctures associated with decreased post-procedural headache
1. In a retrospective review of over 2000 fluoroscopically-guided lumbar punctures and myelograms, the incidence of post-procedural headache was lower than previously reported rates for dural punctures performed without fluoroscopic guidance.
2. In multi-variate analysis, a significant increase in the incidence of headache was associated with young females, and there was no improvement in rates of complication when patients were observed beyond 2-hours of post-procedural bed rest.
Evidence Rating Level: 3 (Average)
Study Rundown: Post-lumbar puncture headaches are common procedure-associated complications due to cerebrospinal fluid (CSF) leakage causing postural intracranial hypotension. Treatment for post-lumbar puncture headache is generally supportive, with varying lengths of prescribed bed rest, analgesia, and in severe cases, tamponade of the puncture site with a blood patch. The reported incidence of post-procedure headache ranges from 5% to 37%, however, this data only applies to dural punctures performed without fluoroscopic image guidance at the bedside. The purpose of this retrospective review is to determine the incidence of post-dural puncture headache in patients that undergo fluoroscopic-guided procedures for either lumbar puncture or myelography.
The study retrospectively analyzed the incidence of post-procedural complications of over 2000 fluoroscopically-guided lumbar punctures and myelograms. At the conclusion of the study, the rate of any post-procedural complication up to 72 hours after the procedure was 2.6%, with a post-dural puncture headache incidence of 2.2%. In multi-variate regression analysis, younger women were significantly associated with an increased incidence of post-procedural headache. Furthermore, there was no significant improvement in the rate of complications among patients prescribed post-procedural bed-rest beyond 2 hours. The results of this study support the hypothesis that fluoroscopically-guided dural punctures may result in decreased rates of post-procedural headaches as compared to traditionally performed punctures. Additionally, the results of this study support the use of a two-hour cut-off for bedrest in the prevention of post-dural puncture complications. The study is strengthened by the use of a single operator to perform all procedures, which reduces operator variability. However, the study is limited by its retrospective nature and the lack of randomization or concomitant arm in which punctures were performed without image guidance, reducing the external validity and generalizability of this study. Additional prospective or randomized controlled trials are needed to confirm this association.
Click to read the study in AJR
Relevant Reading: Post-dural puncture headache: pathogenesis, prevention and treatment
In-Depth [retrospective cohort]: This study was a retrospective review of departmental databases for all patients that underwent outpatient fluoroscopically guided myelograms or lumbar punctures between 2009 and 2014 at a single institution in the United States performed by a single operator. Exclusion criteria included patients undergoing thoracic or cervical punctures. All procedures were performed by a trained radiology practitioner assistant supervised by neuroradiologists. The outcomes of interest were the incidence of headache and other complications 48 to 72 hours post-procedure. Overall, 2,141 procedures were reviewed. At the conclusion of the study, the incidence of any post-procedural complaint and post-procedural headache was 2.6% (95% CI: 2.0% to 3.4%) and 2.2% (95% CI: 1.7% to 3.0%), respectively. Of the cohort that reported headaches, 38% required an epidural blood patch due to severity of symptoms. In multi-variate regression analysis, younger women demonstrated a statistically significant association with increased incidence of post-dural puncture headache. There were no significant associations with needle caliber, driving distance post-procedure, or length of post-procedural bed rest beyond 2 hours.
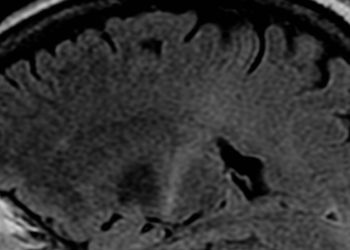
Image: CC/BlausenGallery2014/wiki
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.

![The ABCD2 score: Risk of stroke after Transient Ischemic Attack (TIA) [Classics Series]](https://www.2minutemedicine.com/wp-content/uploads/2013/05/web-cover-classics-with-logo-medicine-BW-small-jpg-350x250.jpg)