Fondaparinux effective as antithrombotic therapy in NSTEMI
1. Fondaparinux had a lower risk of in-hospital and post-hospitalization bleeding events and death compared to low molecular weight heparin (LMWH) treatment.
2. There was no difference in recurrence of myocardial infarction and stroke between the two groups.
Evidence Rating Level: 1 (Excellent)
Study Rundown: In 2007, based on the prior OASIS-5 study, the European Society of Cardiology recommended fondaparinux as the first-choice anticoagulant to treat patients who presented with an NSTEMI. This study was a prospective cohort study performed in Sweden from 2006-2010 that looked at the outcomes of patients with NSTEMI who received LMWH versus fondaparinux as antithrombotic therapy during their hospitalizations.
The study showed that fondaparinux was associated with lower rates of in-hospital death and bleeding as well as in follow-up to 180 days post-hospitalization. There was no difference seen between fondaparinux and LMWH for risk of recurrent MI and stroke up to 180 days post-hospitalization. The strength of the study lies in its population-based design. Weaknesses of the study include its observational design, which limits its ability to determine causality and makes it subject to confounding. However, the study did account for variables such as baseline kidney function, past cardiac history, and history of prior cardiac interventions. In summary, this study supported the findings of the OASIS-5 study and supports the use of fondaparinux in patients with NSTEMI.
Click to read the study, published today in JAMA
Relevant Reading: Comparison of Fondaparinux and Enoxaparin in Acute Coronary Syndromes
In-Depth [prospective cohort]: This study is a prospective cohort study that included 40,616 patients from 2006-2010 in Sweden who were treated either with LMWH or fondaparinux as antithrombotic therapy for an NSTEMI. All patients above 18 were included with no exclusions based on past medical history. However, odds ratios for risk were adjusted for baseline characteristics that included renal function as well as history of coronary arterial disease intervention (e.g., percutaneous and surgical interventions). Outcome measures included in-hospital severe bleeding events and death, 30- and 180-day major bleeding events, death, stroke, and recurrent myocardial infarction (MI). The rate of severe in-hospital bleeding events was lower in the fondaparinux group (OR 0.54, 95%CI 0.42-0.70). This group also was also found to have a lower risk of bleeding or death at 30- and 180-days post-hospitalization (OR 0.74, 95%CI 0.65-0.84; OR 0.72, 95%CI 0.65-0.80, respectively). The fondaparinux group also had a lower risk of death post-hospitalization both at 30 and 180 days. There was no difference in MI or stroke recurrence between the two groups.
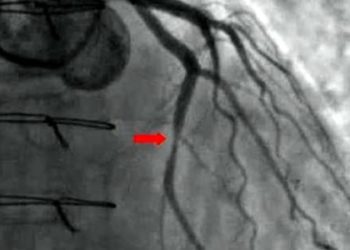
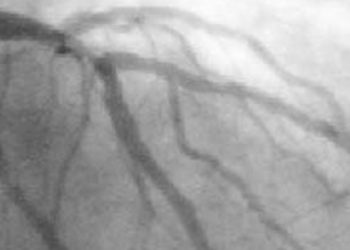
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.