Functional impairment associated with hospital readmission in Medicare seniors
1. Functional impairment, and reduced ability to do activities of daily living, was a risk factor for hospital readmission in Medicare beneficiaries.
2. Hospital readmissions lead to increased health care costs and diminished patient outcomes.
Evidence Rating Level: 2 (Good)
Study Rundown: Hospital readmissions are used as a quality metric, as they are associated with costs to the patient, their family and support system, and society at large. This study sought to more clearly define risk factors for readmission, particularly functional status. The authors selected this factor as many Medicare beneficiaries suffer from some impairment in functional status, and this in turn may be associated with morbidity and mortality. Functional impairment has been studied previously, and is thought to predispose elderly patients to readmission. This study sought to further define this relationship through analysis of a prospective cohort over 10 years.
The authors found a progressive increase in the adjusted risk of readmission (within 30 days from an original hospital admission) as the degree of functional impairment increased. Strengths of the study include the high survey response rate achieved by the Health and Retirement Study, reporting 80-90% response rate. The authors also defined their outcomes to mirror the Center for Medicare Services readmission policies. However, at the same time, the study is limited by reliance on survey data and Medicare claim data. This study suggests that functional impairment may be a worthwhile variable in calculating risk of readmission, and a potential target for intervention.
Click to read the study, published today in JAMA Internal Medicine
Relevant Reading: Rehospitalizations among Patients in the Medicare Fee-for-Service Program
In-Depth [prospective cohort]: This study was part of the Health and Retirement Study (HRS). Specific inclusion criteria for this study included age over 65 years, hospitalization within the study period at an acute care hospital. Admissions for transition to HMO plan within 30 days of discharge, death within 30 days of discharge, transfer to another acute-care facility before discharge, and AMA discharge were excluded. Follow-up surveys were sent every two years. Two measures of functional impairment were used, including the activities of daily living scale (ADL), which measures self-care activities such as bathing, dressing, toileting and eating, and instrumental ADL, which measures such things as managing finances, preparing meals, and using the telephone. Both were obtained from interviews and survey responses.
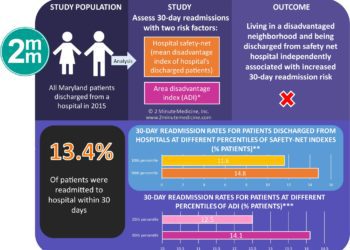
The main outcome studied was readmission within 30 days of discharge. Overall 15.5% of hospitalizations were followed by a 30-day readmission. There was a progressive increase in the adjusted risk of readmission as the degree of functional impairment increased: 13.5% with no functional impairment, 14.3% with difficulty with 1 or more instrumental activities of daily living (OR 1.06; 95%CI 0.94-1.20), 14.4% with difficulty with 1 or more ADL (OR 1.08; 95%CI 0.96-1.21), 16.5% with dependency in 1 to 2 ADLs (OR, 1.26; 95%CI 1.11-1.44), and 18.2% with dependency in 3 or more ADLs (OR 1.42; 95%CI 1.20-1.69).
More from this author: Early removal from neglect may promote normal white matter development, Methadone use for non-cancer pain associated with increased mortality, Criminal behavior more associated with frontotemporal dementia than Alzheimer disease, “No Evidence of Disease Activity” may be useful goal in multiple sclerosis
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.