Geographic variation in rates of antibiotic use: where you live matters
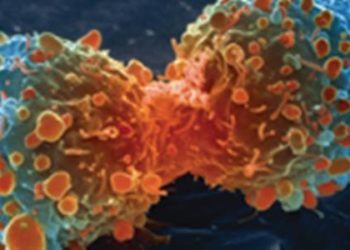
Image: CC/J. Kleyn
Key findings:
1. There is substantial variation in antibiotic prescription rates between geographic regions and between quarterly intervals
2. Policy implications include targeting areas with higher rates of antibiotic use when creating programs to improve prescribing practices.
Primer: Inappropriately prescribing antibiotics results in increasing antimicrobial resistance, greater risks of side effects to patients, and unnecessary costs of medications. Older adults and other vulnerable populations may be more affected by these outcomes, as they may be more susceptible to side effects or more medically complex. Factors contributing to overuse of antibiotics include physicians who prescribe them in the wrong instances (e.g. prescribe antibiotics for viral infections, or prescribe a broad-spectrum antibiotic where a narrow-spectrum antibiotic is sufficient), prescribe an inappropriate dose or duration, and patients who insist on being prescribed antibiotics. Studies have investigated the types of programs and methods of intervention that may improve prescribing practices; however, the application of this research requires guidance as to when and where these interventions will be most useful.
For further reading, please see the following studies:
This [retrospective cohort] study: This study, published in JAMA, analyses three years of prescription drug data from the Centers for Medicare & Medicaid Services for beneficiaries 65 years and older. Differences in rates of antibiotic use were examined between quarterly intervals and also at three levels of geographic distribution: hospital referral regions, states and the District of Columbia, and national regions (South, West, Midwest and Northeast). Outcomes of proportion of patients using an antibiotic, mean number of antibiotic prescriptions filled, and mean total gross spending on antibiotics were measured per person per year or per person per quarter. There was a significant difference in rates of antibiotic use between geographic regions with the highest rate observed in the South and the lowest rate in the West (P<0.01). There was also a significant difference in the rate of antibiotic use between quarters with the highest rate occurring in the first quarter and the lowest in the third quarter (P<0.1).
In sum: There was substantial variation in the use of antibiotics between geographic regions and between quarterly intervals and this was shown to be independent of differences in prevalence of disease. This variation in antibiotic prescription was larger than what has been observed in previous studies that examined patterns of use of all medications.
Although there were adjustments for patient characteristics such as demographics and insurance status, it was not possible to fully adjust for factors such as specific requests for antibiotics or disease severity. This may contribute to the large variation observed.
Overall, the results suggest particular regions of higher antibiotic use which may be targeted by programs and interventions to reduce inappropriate prescription of antibiotics.
Click to read in the Archives of Internal Medicine
Written by AdC and AC
© 2012 2minutemedicine.com. All rights reserved. No works may be reproduced without written consent from 2minutemedicine.com. DISCLAIMER: Posts are not medical advice and are not intended as such. Please see a healthcare professional if you seek medical advice.

![PFO closure equivalent to medical management in prevention of recurrent stroke [PC and RESPECT trials]](https://www.2minutemedicine.com/wp-content/uploads/2013/03/Echokardiogram_von_Atriumseptumdefekt_Ostium_secundum1-350x250.jpg)