Greater thoracic aortic aneurysm size associated with worse long-term outcomes
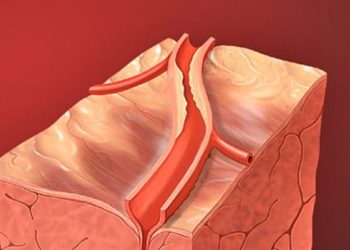
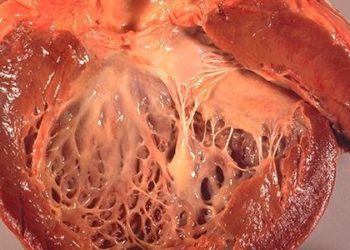
1. There is a positive relationship between adverse events, including aortic dissection (AD) and all-cause death, and initial transthoracic aortic aneurysm (TAA) size, which dramatically increases with an initial TAA size of 6.0 cm or greater.
2. Overall, the rate of AD was low in this study, but was significantly greater in patients with an initial TAA size 6.0 cm or larger than in patients with a smaller initial TAA size.
Evidence Rating Level: 2 (Good)
Study Rundown: Ascending transthoracic aortic aneurysms (TAA) can predispose patients to aortic dissection (AD), a possibly fatal event with high rates of mortality. Given the limitations of previous research, there is controversy regarding the appropriate size of the prophylactic aortic intervention, and current guidelines are based on limited evidence. These guidelines vary over time, with changing thresholds for TAA size for operative intervention, and are not supported by evidence from high-quality clinical trials. This study aims to examine the natural history of TAA, including the risks of AD, death, and surgical intervention. Data was examined from a large integrated healthcare delivery system (Kaiser Permanente Northern California [KPNC]) from 2000 to 2016. In total, 6372 patients were retrospectively identified that met the inclusion criteria for this research. With respect to the primary outcomes, the overall unadjusted rate of AD was quite low, only occurring in 44 patients (0.7%), with an overall incidence of 0.22 per 100 person-years. Of note, there were no AD events in patients with an initial TAA size of 4.0 cm or smaller, and the overall rate of AD in patients with an initial TAA size smaller than 6.0 cm was less than 0.5 per 100 person-years. However, in patients with an initial TAA size 6.0 cm or larger, the rate of AD was 2.19 events per 100 person-years. In addition, the composite rate of AD or all-cause death was positively associated with increasing TAA size, though was notably higher for those with an initial TAA size of 6.0 cm or larger. Furthermore, rates of elective surgery also increased with a larger initial TAA size. Using a multivariable model controlling for other associated risk factors, initial TAA size was independently associated with an increased risk of AD. Adjusted hazard ratios (HRs) for the risk of AD were increased in patients with initial aortic sizes 4.5 to 4.9 cm relative to 4.0 to 4.4 cm. There was no statistically significant difference in the HRs for initial aortic size of 5.0 to 5.4 cm and 5.5 to 5.9 cm, but the HR increased for patients with an initial TA size of 6.0 cm or larger. Overall, though the overall rate of AD in this study was quite low, a larger initial TAA size is associated with a higher risk of AD and all-cause death after adjusting for potential co-founders, with a dramatic increase at 6.0 cm or larger. The findings from this study support the current guidelines recommending prophylactic surgery at 5.5 cm given the increased adverse events in patients with an initial aortic size of 6.0 cm or larger. A major limitation of this study is that patients who received prophylactic aortic surgery would be removed from the risk pool, which causes underreporting of adverse events, especially in those with larger initial TAA sizes. This study is one of the largest natural history studies for TAA and is an important step to gather evidence for the guideline recommendations about prophylactic aortic surgery, especially since the surgery itself is associated with many risks of its own. Overall, this retrospective cohort study suggests an association of initial TAA size with adverse outcomes including AD and all-cause death, with a dramatic increase of these risks at an initial aortic size of 6.0 cm or larger.
Click to read the study in JAMA Cardiology
Relevant Reading: What is the appropriate size criterion for resection of thoracic aortic aneurysms?
In-Depth [retrospective cohort study]: This study analyzed the relationship of TAA size with AD events, all-cause death, and surgical intervention in patients with a documented TAA size in the KPNC database. Included were patients with an imaging study documenting TAA 3.5 cm or larger, patients 18 years or older, and patients without any prior AD or aortic surgery. Excluded were patients with a predisposition to TAA. With respect to population characteristics, the mean age of patients was 68.8, and there were approximately twice as many male individuals than female individuals in each category; in the total cohort, there were 2050 (32.2%) female individuals and 4322 (67.8%) male individuals. There were a significant number of patients in each initial TAA size category, with 828 patents (13.0%) with TAA size 5.0 cm or larger, and 280 (4.4%) with TAA size 5.5 cm or larger at diagnosis. With respect to the primary outcome, unadjusted rates of AD were low and only occurred in 44 (0.7%) patients across the cohort, representing 0.22 (95% CI, 0.15-0.28) per 100 person-years. However, when stratified by initial TAA size, there were no AD events in those with an initial TAA size of 4.0 cm or smaller, and in those with an initial TAA size of 6.0 cm or larger, the rate was 2.19 events per 100 person-years. Similarly, the rates of all-cause death were much higher in patients with an initial TAA size of 6.0 cm or larger. Elective surgery was also more common in patients with larger initial TAA sizes. Using multivariable models controlling for confounding risks, the adjusted HR for the risk of AD increased for an aortic size of 4.5 to 4.9 cm (HR, 2.37; 95% CI, 1.17 – 4.81) when compared to the initial TAA size of 4.0 to 4.4 cm. HRs for initial TAA size of 5.0 to 5.4 cm and 5.5 to 5.9 cm were not statistically significant, but the HR was much higher in patients with initial TAA size of 6.0 cm or larger (HR, 11.09; 95% CI, 3.05 – 40.36).
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.