Human donor milk equivalent to preterm formula for neurodevelopment in very-low-birth-weight infants
1. There were no statistically significant differences when comparing nutrient-fortified human donor milk with preterm formula on cognitive, language or motor composite scores among very-low-birth-weight infants. Similarly, there were no differences in morbidity, mortality, or growth scores.
2. Improved neurodevelopment should not be a treatment goal when using donor milk in the setting of high provision of mother’s milk.
Evidence Rating Level: 1 (Excellent)
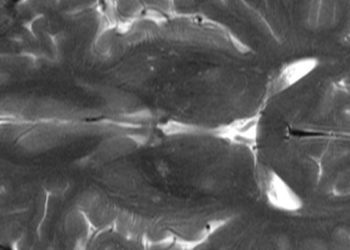
Study Rundown: Very-low-birth-weight (VLBW) infants benefit from a diet of their mother’s milk, showing reduced rates of comorbidities like necrotizing enterocolitis, late-onset sepsis, and poor neurodevelopment. Donor human milk or preterm formula are often used in these infants when mother’s milk is not available in sufficient quantity. While previous studies have raised awareness of possible gains in growth from using preterm formula compared to donor milk, current evidence is limited in identifying the clear risks and benefits of “nutrient-fortified” human donor milk.
In this study, the effects of nutrient-enriched donor milk and preterm formula as a supplement to mother’s milk were evaluated in VLBW infants. Infants were randomized to one of the two supplements for 90 days or until discharge from the hospital, and were followed-up until 18 months of age. The study found no statistically significant differences across the feeding interventions with regards to neurodevelopment nor morbidity or mortality.
Overall, this study suggests no significant differences between nutrient-fortified donor milk and formula milk in improving neurodevelopment in VLBW infants. Further, when using nutrient-fortified donor milk in the setting of high provision of mother’s milk, improved neurodevelopment should not be a treatment goal. Limitations of the study include the unclear predictive validity of neurodevelopment measures, and, notably, follow-up assessments of neurocognitive function for each participant is planned at 5 years of age. What’s more, the lack of apparent differences may be due, in part, to the high provision of mother’s milk available in the NICU during this study, which may have mitigated any effects of the supplementation.
Click to read the study, published today in JAMA
Relevant Reading: Randomized Trial of Donor Human Milk Versus Preterm Formula as Substitutes for Mothers’ Own Milk in the Feeding of Extremely Premature Infants
In-Depth [randomized clinical trial]: This double-blind, randomized control trial enrolled VLBW infants between October 2010 and December 2012 from 4 tertiary care neonatal intensive care units in Southern Ontario, Canada. Eligibility criteria included birth weight less than 1500 g with enteral feeding starting within 7 days of birth. Mother’s milk was fed to the infants whenever available, however if not available, infants were randomized to receive nutrient enriched donor milk or preterm formula for 90 days or until discharge from the hospital. A cognitive composite score comprised the primary outcome and was obtained at 18 months’ corrected age using the Bayley Scales of Infant and Toddler Development, Third Edition. Language and motor composite scores, mortality and morbidity index, and growth during feeding intervention comprised the secondary outcomes. Morbidities included late-onset sepsis, necrotizing enterocolitis, chronic lung disease, and retinopathy of prematurity. The study found no significant differences in cognitive, language, or motor composite scores, nor in mortality or morbidity. Post-hoc exploratory analysis, however, showed more participants in the donor milk group having cognitive composite scores indicative of neuro-impairment compared with infants receiving preterm formula (p = 0.02). Preplanned exploratory analysis suggested feeding donor milk as a supplement was associated with a lower risk of necrotizing enterocolitis.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.