Imaging of atherosclerotic inflammation possible with fluorine MRI
1. The use of an injectable fluorinated carbohydrate during magnetic resonance imaging allowed for identification and quantification of macrophage foam cells in a mouse model of atherosclerosis, providing proof-of-concept for a high-resolution imaging evaluation of atheromatous inflammation.
Evidence Rating Level: 2 (Good)
Study Rundown: Atherosclerotic plaque is the fundamental lesion underlying the many manifestations of cardiovascular disease, the leading cause of death in the United States. Plaque evaluation by computed tomography and magnetic resonance (MR) imaging has been effectively used for years to characterize a patient’s plaque burden and makeup. However, these techniques do not provide any information regarding the underlying inflammatory process, which is known to be a more specific predictor of future plaque rupture or other atherosclerosis-related sequelae than structure alone. Qualitative imaging of plaque inflammation has previously been achieved using various techniques such as iron oxide particles and PET imaging, but these methods are limited by toxicity, cost, and poor signal-to-noise ratios. In the current proof-of-concept study, the authors utilized MR imaging using 19F in perfluorocarbons (PFCs) to assess plaque inflammation in a mouse model of atherosclerosis. They hypothesized that the relative lack of biologic fluorine would provide a low background signal to facilitate quantitation over time, while the fluorocarbons themselves would be actively taken up by foam cells within a region of active plaque inflammation to allow highly specific, direct plaque visualization. Test animals were imaged at several time points following PFC injection and histologic correlation was performed to ensure specificity of the imaged fluorine signal. The results suggested that fluorine signal following PFC injection strongly correlates with regions of inflammation underlying atherosclerotic plaques. This signal persisted over several days, allowing for delayed and quantitative assessment of disease progression. The study was limited in that a lack of quantification of total injected PFCs limited assessment of the true sensitivity of the study in determining the lower threshold of cellular uptake necessary for resolvable signal. Additionally, the nature of animal studies limits the direct translation to human trials.
Click to read the study in Radiology
Relevant Reading: Inflammation in atherosclerosis
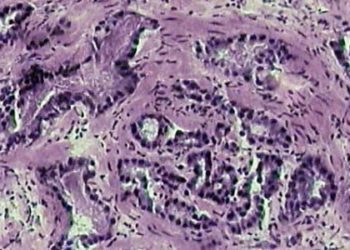
In-Depth [animal study]: Apolipoprotein E knockout mice fed a high-fat diet for atherosclerotic acceleration underwent serial injections of a carbohydrate emulsion enriched with 19F, followed by serial MR imaging at 9.4 Tesla. A separate control group was similarly imaged following injection of sterile saline. All generated images were evaluated by one experienced reader. Study animals were then sacrificed and the aorta and branch vessels were sectioned for histopathologic correlation of the imaging findings. The MR imaging results demonstrated a tropism of the injected PFCs for atherosclerotic plaque within the aortic arch, carotid arteries, and brachiocephalic artery, as well as for areas of high immune cell density such as lymph nodes. No aortic PFC signal was detected in any control animals. The PFC signal-to-noise ratio (SNR) rose daily and peaked at day six (mean SNR 13.4 ± 3.3). Histopathologic evaluation demonstrated excellent correlation between PFC signal and inflammatory atherosclerotic plaque within the aorta and branch vessels, particularly within foamy macrophages. These findings were further confirmed by immunofluorescent staining for PFC. No histopathologic evidence of uptake was noted in control mice.
More from this author: Dual-energy CT may improve detection of acute small bowel ischemia, Pancreatic cancer screening with MRI may benefit high-risk patients, Quantitative MRI may differentiate true from pseudoprogression in glioblastoma, MR lymphangiography useful for evaluation of central lymphatic pathology
Image: PD
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.