Impact of frailty on clinical outcomes and resource use following emergency general surgery in the United States
1. Following emergency general surgery procedures, frail patients had poorer clinical outcomes such as higher mortality, non-home discharge rates, and hospital readmissions, as well as greater hospital costs.
Evidence Rating Level: 2 (Good)
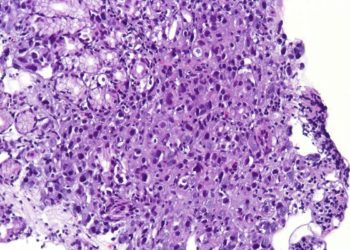
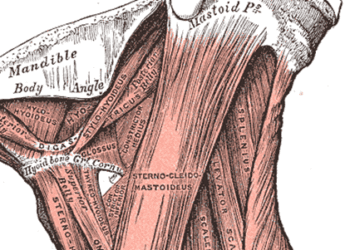
Emergency general surgeries (EGS) carry greater risk of mortality and other poorer clinical outcomes, due to the involvement of patients in critical states, such as organ dysfunction and compromised physiology. Although old age has been found to unreliably predict poorer postsurgical outcomes, frailty is a potential predictor. Frailty refers to patients with many chronic conditions who cannot tolerate physiologic stresses. The current retrospective study evaluated the association of frailty with clinical outcomes such as mortality length of stay, hospital costs, non-home discharge rates, and readmissions, following EGS operations. The study population was taken from the nationwide Readmissions Database (NRD), which accounts for 58% of all hospitalizations in the USA. Patients were included for EGS procedures, such as large and small bowel resection, perforated ulcer repair, cholecystectomy, and appendectomy. The Johns Hopkins frailty index was used to separate patients into frail and nonfrail groups: Frailty diagnoses included dementia, vision impairment, weight loss, poverty, and lack of access to healthcare. Overall, the study population consisted of 655,817 patients, of which 78,093 (11.9%) were categorized as frail. This cohort was older, with 65.0% being older than 65 years, compared to 32.4% in the nonfrail cohort. The study found that the frail cohort had higher rates of mortality, non-home discharge, hospital readmission, and hospital costs. Perforated ulcer repair and large bowel resection were the procedures with the greatest differences in mortality rate. With regards to mortality rate, the greatest difference was found for perforated ulcer repair (8.3%, 95% CI 7.1-10.4%). For non-home discharge, perforated ulcer repair and large bowel resection exhibited the largest differences. And for hospital costs, perforated ulcer repair showed the greatest differences ($24,600, 95% CI $22,300-26,900). Therefore, this study found that frail patients had poorer clinical outcomes and increased use of medical resources after EGS, which underlies the need for using frailty assessments to identify patients, to provide optimal support postoperatively.
Click to read the study in PLOSONE
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.