Improving immune activity may decrease Alzheimer’s disease pathology [PreClinical]
1. In a mouse model of Alzheimer’s disease (AD), blocking the programmed death-1 (PD-1) pathway with anti-PD-1 antibody treatment increased the population of infiltrating myeloid cells in the brain.
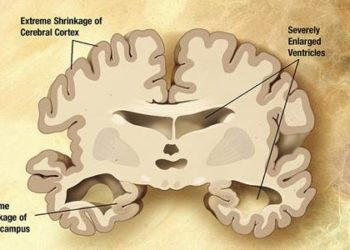
2. Mice that received two rounds of anti-PD-1 antibody treatment showed improved memory and clearance of amyloid-β plaques in the hippocampus and cerebral cortex regions.
Evidence Rating Level: 2 (Good)
Study Rundown: Alzheimer’s disease is a condition that is marked by progressive memory loss and the formation of amyloid-β (Aβ) plaques in the brain. Though neurodegenerative diseases such as AD often exhibit neuroinflammation, the anti-inflammatory drugs tested to date have been unsuccessful in improving disease symptoms. In this work, the authors instead increased immune system activity through anti-PD-1 antibody treatment as a means of treating AD.
Using the five familial AD mutations (5XFAD) mouse model of AD, the researchers demonstrated that administration of PD-1 blocking antibody increased the presence of myeloid cells in the brain relative to IgG control treatment. Anti-PD-1-treated animals with advanced stage pathology exhibited improved memory, as determined by the decrease in the number of errors made during the radial arm water maze (RAWM) test. When mice were given two rounds of anti-PD-1, their performance in the test improved over those given only a single treatment round. Subsequent histological analysis of brain sections revealed a decrease in the number and size of Aβ plaques in the antibody-treated cohorts. These plaque reduction results were confirmed using a second mouse model of AD, APP/PS1 mice, which develops more severe manifestations of the disease.
This work highlights the potential to blockade the PD-1 immune checkpoint pathway as a treatment for AD. Currently, various anti-PD-1 treatments are being tested and used for the treatment of cancer. Encouraging safety and toxicity studies in cancer patients provide promise in using PD-1 blocking antibodies as a method of treating AD and other neurodegenerative diseases.
Click to read the study in Nature Medicine
Relevant Reading: IFN-γ-dependent activation of the brain’s choroid plexus for CNS immune surveillance and repair
In-Depth [animal study]: C57/BL6-SJL mice with the 5XFAD transgenes were treated with 2 intraperitoneal injections of anti-PD-1 antibody (n=5) or IgG control (n=4) at 250 μg/animal. One week after treatment, the proportion of infiltrating myeloid cells present in the brain was measured by flow cytometry (CD45highCD11b+). The anti-PD-1 group showed a significant increase relative to control (p<0.05). These immune cells were found to also express scavenger receptor A (SRA1), a receptor involved in the clearance of Aβ plaques.
To assess the impact of treatment on memory and spatial learning, the RAWM test was used. Briefly, a water tank contained 6 compartments radiating out from the center, with a submerged escape platform at the end of one compartment. Mice were trained to find the platform on day 1 and tested on day 2. 10-month-old mice were tested one month after a single anti-PD-1 treatment. Compared to the IgG control group (n=6), the treatment group (n=9) performed with significantly fewer errors after 4 trials of testing (p<0.001). When mice received 2 rounds of treatment, each separated by one month, performance was improved to levels comparable to the wild-type, healthy control cohort. Histology of the hippocampus and layer V of the cerebral cortex showed that both treatment schemes resulted in significant decreases in Aβ plaque number and size (percent of tissue area positively stained for Aβ).
These results were confirmed in a second, more aggressive model of AD. APP/PS1 mice, aged 8- and 15-months (n=4 per group), were treated with a single round of anti-PD-1 and examined one month later. Anti-PD-1 treatment led to fewer and overall smaller plaques (p<0.01).
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.