Increased body mass index in teens linked to risk of colorectal cancer
1. Adolescent body mass index (BMI) was associated with a statistically significant increased risk of colorectal cancer (CRC).
2. Inflammation in adolescence, as measured through erythrocyte sedimentation rate (ESR), was also associated with increased risk of CRC.
Evidence Rating Level: 2 (Good)
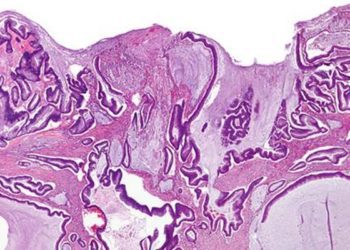
Study Rundown: Colorectal cancer is the third most common cancer among men and women and the third most common cause of death due to cancer in the United States. BMI has been linked to CRC risk, but little is known about the effect of adolescent obesity on CRC risk. The purpose of this study was to determine whether BMI and ESR levels during adolescence impacted the risk of CRC in a group of nearly 240,000 Swedish men. Compared to normal weight adolescents (BMI 18.5-24.9), those who were upper overweight (BMI 27.5-29.9) had an over 2 times greater risk of CRC, while those who were obese (BMI 30+) had a nearly 2.4 times risk of CRC. For inflammatory levels, male adolescents with ESR >15 had an over 60% higher risk of CRC compared to those with low ESR <10.
This study benefited from utilizing a large population-based cohort of patients that allowed the authors to evaluate the relationship between BMI, inflammation, and CRC risk. However, the data are only from men and it’s possible that obesity and inflammation have differing roles in women and on their risk of CRC. Additionally, BMI and ESR were only assessed in adolescence and not again later in life. Thus, it’s possible these men’s weight and inflammatory levels changed later in life and positively or negatively influenced their risk of CRC. Overall, this study suggests that weight and inflammation may play important roles in the development of CRC, and that there are still many downstream benefits of tackling the childhood obesity epidemic.
Click to read the study in Gut
Relevant Reading: Measured body mass index in adolescence and the incidence of colorectal cancer in a cohort of 1.1 million males
In-Depth [retrospective cohort]: This study looked to determine what effects ESR levels, as an indicator of inflammatory levels, and BMI had on future risk of CRC. At the time that Swedish men underwent compulsory conscription assessment for the military between 1969-1976, an extensive standardized physical assessment was performed. These 239,658 men were followed for CRC using the Swedish Cancer Registry, and over an average of 35 years of follow-up, 885 diagnoses of CRC were made. Patients with IBD, history of CRC, and ill-defined health problems were excluded from the analysis. Compared to normal weight adolescents (BMI 18.5-24.9), those who were upper overweight (BMI 27.5-29.9) had a 2.08 times greater risk (CI95% 1.40-3.07) of CRC, while those who were obese (BMI 30+) had a 2.38 times risk (CI95% 1.51-3.76) of CRC (p-trend <0.001). After multivariable adjustment, moderately elevated ESR (10-14.9) was associated with a 40% increased risk of CRC compared to normal ESR (<10), though this was non-significant (CI95% 0.93-2.10). Male adolescents with high ESR >15 had a 63% higher risk of CRC (CI95% 1.08-2.45) (p-trend 0.006).
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.