Increased risk of mortality and epilepsy in individuals post-stroke
1. In this cohort study, it was found that acute symptomatic status epilepticus is associated with a higher risk of mortality and post-stroke epilepsy as compared to short acute seizures or no seizures.
2. The SeLECT 2.0 calculator, based on a prognostic model, was updated to capture individuals post-stroke with a high risk of epilepsy.
Evidence Rating Level: 2 (Good)
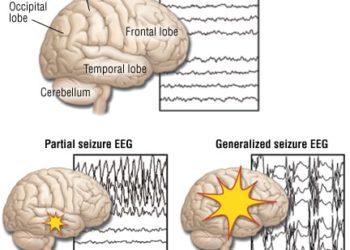
Study Rundown: Stroke contributes to a majority of deaths from neurological disorders and is the leading acquired cause of epilepsy in the elderly. While remote seizures (occurring >1 week after stroke) are considered unprovoked and qualify as post-stroke epilepsy, acute seizures (<1 week after stroke) are considered provoked, do not qualify as epilepsy, and are typically not treated with long-term anti-epileptics. It is unknown whether the various types of acute symptomatic seizures differ in their risks of post-stroke mortality and epilepsy. As such, this study aimed to build upon its prognostic model, SeLECT, using multivariable Cox proportional hazards regression to account for types of acute symptomatic seizure. The results revealed individuals with ischemic stroke and status epilepticus had a higher risk of 10-year mortality and epilepsy (79% and 81%, respectively) compared to those with short acute symptomatic seizures (30%; 40%) and without seizures (11%; 13%). One limitation of the study was that the diagnosis of seizures was reliant upon clinical evaluation and not electroencephalogram (EEG) in all cases. Therefore, the results cannot be generalized to non-convulsive status epilepticus without clinical signs. Nonetheless, this study highlights that acute symptomatic status epilepticus is an indicator of high risk of mortality and epilepsy. Stroke survivors and caregivers should be informed of this risk and monitor accordingly. Clinically, the updated calculator (SeLECT 2.0) can be used to estimate risk of post-stroke epilepsy for stroke survivors.
Click to read the study in JAMA
In-Depth [retrospective cohort]: This study involved a derivation cohort from 9 international tertiary referral centers (with data from 2002 to 2019) and a replication cohort from 3 hospitals in Europe (data from 2002 to 2020). Of the 4552 individuals with acute ischemic stroke in the derivation cohort, 226 (5.0%) patients had acute symptomatic seizures. These were further categorized as status epilepticus in 8 individuals (0.2%), short seizures in 182 (4.0%) and undetermined or unknown type in 36 (0.8%). Acute symptomatic status epilepticus was a significant predictor of all-cause mortality (hazards ratio: 12.7; 95% CI, 3.0-52.7; p<0.001) and epilepsy (HR: 4.3; 95%CI, 1.3-13.9; p<0.02). Short acute symptomatic seizures had a non-significant association for all-cause mortality after correction for pre-stroke disabilities and comorbidities. A replication cohort consisting of individuals with acute symptomatic status epilepticus post-ischemic stroke revealed similar 10-year risks of mortality and epilepsy to the derivation cohort. The prognostic model, SeLECT, was modified to award additional points if an acute symptomatic status epilepticus occurs and can be found on web and smartphone applications for clinical use.
Image: PD
©2023 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.