Intensive blood pressure control significantly reduces vascular risks
1. In this systematic review and meta-analysis, relative risks for vascular events (major cardiovascular disease, coronary heart disease and stroke) were reduced in proportion to systolic blood pressure reductions.
2. Different classes of drugs were not uniform in their efficacy for specific preventions. For example, beta blockers were inferior in preventing major cardiovascular disease events, stroke, and renal failure, whereas calcium channel blockers were inferior in preventing heart failure.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Systolic hypertension is a well-known risk factor for a number of vascular diseases, such as coronary heart disease, stroke, and renal disease. It is the general consensus that pressure reduction is beneficial for patients with vascular risk factors and poorly controlled systolic pressures; however, optimal goals for pressure control have not been firmly established. Recent evidence-based guidelines such as those of NICE and European Society of Hypertension have advocated a more relaxed target of blood pressure control from 130/85 mmHg to 140/90 mmHg, and to 150/90 mmHg for the elderly. In the current systematic review and meta-analysis by Ettehad et al, the investigators pooled data from more than 600,000 participants and identified statistically significant reductions in vascular relative risks proportional to systolic pressure reductions. The reductions held across various baseline blood pressure levels and comorbidities. Another observation was that different classes of drugs were not uniform in their abilities to prevent specific morbidities. Beta blockers were found to be inferior for the prevention of major cardiovascular disease events, stroke and renal failure. Calcium channel blockers were found superior for the prevention of stroke, whereas inferior in preventing heart failure – for which diuretics were superior. Based on the study results, the investigators advocate stricter control guidelines to systolic pressure below 130 mmHg. The study results were strengthened by the large number of patients involved in the analyses, as well as low-to-moderate heterogeneity for outcomes.
The study was funded by National Institute for Health Research and Oxford Martin School.
Click to read the study in The Lancet
Relevant Reading: Age-specific relevance of usual blood pressure to vascular mortality: a meta-analysis of individual data for one million adults in 61 prospective studies
In-Depth [systematic review and meta-analysis]: This systematic review and meta-analysis included 123 trials with 613,815 participants. Eligible trials were identified in MEDLINE from Jan 1, 1966 to July 7, 2015 with search terms related to blood pressure control and drug classes, such as “anti-hypertensive agents” and “thiazide”. 92 studies were deemed to be trials of blood pressure lowering. 43 trials compared different drug classes.
Meta-regression analyses demonstrated relative risk reductions for major cardiovascular disease events (p<0.0001), stroke (p<0.0001), heart failure (p<0.0001), and all-cause mortality (p=0.014). In addition, these reductions were proportional to the magnitude of blood pressure reductions. Every 10 mmHg reduction in systolic blood pressure significantly reduced the risk of major cardiovascular disease events (RR 0.80, 95% CI 0.77-0.83), coronary heart disease (0.83, 0.78-0.88), stroke (0.73, 0.68-0.77), heart failure (0.72, 0.67-0.78), and all-cause mortality (0.87, 0.84-0.91). Of note, stratification by mean baseline systolic pressure resulted in no significant trends for any outcomes between strata.
In comparing the five classes of blood pressure drugs, the different classes were largely similar in effectiveness for preventing various outcomes. However, beta blockers were less efficacious for preventing major cardiovascular disease events (RR 1.17, 95% CI 1.11-1.24), stroke (1.24, 1.14-1.35), and renal failure (1.19, 1.05-1.34). Calcium channel blockers were superior for stroke prevention (0.90, 0.85-0.95), but were inferior for heart failure prevention (1.17, 1.11-1.24). Diuretics were superior for heart failure prevention (0.81, 0.75-0.88).
10 studies were judged to be of unclear risk of bias and 113 were deemed to be at low risk of bias. Heterogeneity for outcomes was low to moderate (I2 statistics for heterogeneity were 41% for major cardiovascular disease, 25% for coronary heart disease, 26% for stroke, 37% for heart failure, 28% for renal failure and 35% for all-cause mortality).
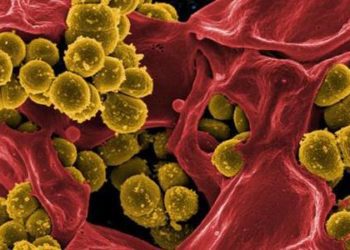
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.