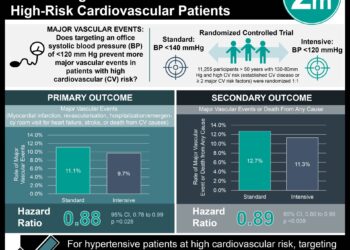
Intensive systolic blood pressure reduction below 140 mmHg reduces risk of major cardiovascular events
1. In this systematic review and meta-analysis of randomized controlled trials, more intensive treatment to lower systolic blood pressure below the currently recommended goal of 140 mmHg significantly reduced the risk of major cardiovascular events, myocardial infarction, stroke, retinopathy progression, and albuminuria, compared to less intensive treatment.
2. Trials in which all patients had vascular disease, renal disease, or diabetes showed the greatest benefit in intensive blood pressure reduction compared to other trials, and the overall effects of intensive treatment were consistent across all major patient subgroups.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Guidelines blood pressure goals in high-risk patient populations have changed over time, with recommendations to increase the target blood pressure for patients with cerebrovascular disease, coronary heart disease, renal disease and diabetes to 140/90 mmHg, and 150/90 mmHg for individuals over age 60. However, a significant number of blood pressure-attributable events occur in patients with a systolic blood pressure below 140 mmHg. This study conducted a systematic review of the literature to assess all trials comparing various blood pressure targets and specifically focus on the safety and efficacy of lowering systolic blood pressure below 140 mmHg in high-risk patients.
The results showed a mean blood pressure level at follow-up of 133/76 mmHg in the more intensive blood pressure treatment group compared to 140/81 mmHg in the less intensive treatment group. More intensive treatment significantly reduced the risk of major cardiovascular events, myocardial infarction, stroke, retinopathy progression, and albuminuria, compared to less intensive treatment. However, there was no significant reduction in the risk of heart failure, cardiovascular death, non-cardiovascular death, end-stage kidney disease, or total mortality. Additionally, trials in which all patients had vascular disease, renal disease, or diabetes showed the greatest benefit in intensive blood pressure reduction, and the overall effects of intensive treatment were consistent across all major patient subgroups. Severe hypotension was associated with more intensive treatment, but no significant serious adverse events were associated with blood pressure lowering in both treatment groups. This study was strengthened by including trials comparing different blood pressure targets and a variety of patient populations, but was limited in that individual participant data was unavailable to analyze treatment effects in various population groups.
Click to read the study in The Lancet
In-Depth [systematic review and meta-analysis]: 19 randomized controlled trials including 44,989 participants were analyzed for this study. 2,496 major cardiovascular events, 1,762 all-cause deaths, and 514 end-stage kidney disease events were observed during a mean follow-up of 3.8 years (range 1.0-8.4 years). The mean baseline blood pressure levels ranged from 123-172 mmHg systolic and 76-105 mmHg diastolic, with an overall mean of 159/92 mmHg. The mean follow-up blood pressure levels were 133/76 mmHg in the more intensive treatment groups and 140/81 mmHg in the less intensive treatment groups.
Intensive blood pressure lowering treatment compared to less intensive treatment reduced the risk of major cardiovascular events by 14% (95% CI 4-22), myocardial infarction by 13% (0-24), stroke by 22% (10-32), retinopathy progression by 19% (0-34), and albuminuria by 10% (3-16). However, no significant reduction was observed with more intensive treatment in reducing the risk of heart failure (Relative Risk [RR] 0.85, 95% CI 0.66-1.11), cardiovascular death (0.91, 0.74-1.11), non-cardiovascular death (0.98, 0.86-1.13), end-stage kidney disease (0.90, 0.77-1.06), or total mortality (0.91, 0.81-1.03). Trials in which all patients had vascular disease, renal disease, or diabetes had an average control group rate of major vascular events of 2.9% per year compared to 0.9% in other trials, resulting in a number needed to treat of 94 (95% CI 44-782), compared to 186 (107-708) in all other trials. Six trials reported serious adverse events, with five trials reporting an increased risk of severe hypotension with intensive treatment (61 events [0.3% event rate per person-year]) compared to less intensive treatment (23 events [0.1%]; p=0.015), but there were no significant serious adverse events associated with blood pressure lowering (280 events [1.2%] vs. 211 events [0.9%], p=0.112).
Image: PD
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.