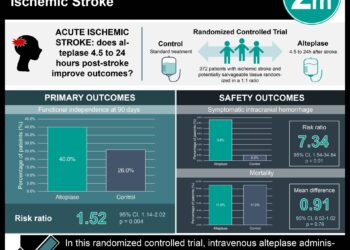
Intraarterial therapy improves outcomes in acute ischemic stroke
1. Patients with confirmed occlusion of a proximal intracranial artery who underwent intraarterial treatment in addition to the typical alteplase treatment had improved functional outcomes at 90 days, as measured by the modified Rankin scores, when compared to similar patients undergoing intravenous alteplase therapy alone.
2. There was no significant difference in adverse outcome rates between the two trial arms, including mortality and symptomatic intracerebral hemorrhage.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Though catheter-based intraarterial stroke therapy has been used in clinical practice for several years, there has been an historical lack of evidence in favor its utilization. The simultaneous publication of three equivocal or negative trials evaluating the technique in 2013 raised concerns over its widespread use, though those trials were widely criticized for their methodologic weaknesses. In the present study—the Multicenter Randomized Clinical Trial of Endovascular Treatment for Acute Ischemic Stroke (MR CLEAN)—a large group patients from multiple clinical sites in the Netherlands with acute ischemic stroke were randomized to either intraarterial treatment or standard medical therapy. All patients had intracranial arterial occlusion at the time of enrollment, confirming their potential eligibility for intraarterial therapy. The results showed significantly improved clinical outcomes at 90 days among patients treated with intraarterial therapy as measured by the modified Rankin scale score. The MR CLEAN investigators did not identify any significant difference in the rate of adverse outcomes in the two groups, including mortality and intracerebral hemorrhage. The principal limitations of the study were heterogeneity within the treatment arm, which included variability in the type of intraarterial therapy administered and the simultaneous revascularization of the cervical carotid artery in some patients, which may have limited the generalizability of results. Another limitation included relatively lower rate of reperfusion (58%) with intraarterial treatment when compared to prior reported values of greater than 80%. Future studies could expand on these findings by increasing the total number of patients enrolled, allowing for further evaluation of the applicability of intraarterial treatment in more distal intracranial lesions.
Click to read the study in NEJM
Relevant Reading: Endovascular Treatment for Acute Ischemic Stroke
In-Depth [randomized controlled trial]: In this multicenter, randomized controlled trial, 500 patients with acute ischemic stroke and radiographic evidence of large vessel occlusion were enrolled. Eligible patients who presented within 6 hours of symptom onset were randomized to receive intraarterial stroke therapy in addition to routine alteplase therapy or routine medical care alone. Intraarterial therapy was defined as directed intraarterial thrombolysis, mechanical thrombectomy, or both treatments together. A total of 445 patients received intravenous alteplase before randomization, and 233 patients were randomized to the intraarterial intervention group. Of these 233, 190 (81.5%) underwent treatment with retrievable stents, while others received treatment with a different device, and 24 patients received additional intraarterial thrombolytic agents. The primary outcome was the score on the modified Rankin scale at 90 days, which showed an adjusted common odds ratio of 1.67 (CI95%, 1.21-2.30) for the intervention arm. There was an absolute difference in the proportion of patients who had a modified Rankin score of 0-2 (functionally independent) of 13.5 percentage points (CI95%, 5.9-21.2) and an adjusted odds ratio of 2.16 (CI95%, 1.39-3.38) between the intervention (32.6% with Rankin score of 0-2) and control arm (19.1% with Rankin score 0-2). A total of 141 of the 187 patient showed absence of residual occlusion in the intervention group compared to 68 of 207 patients in the control group. There was no significant different between group in adverse events at 90 days (p=0.31), but it was noted that 13 of the 233 in the intervention arm did develop signs of a new ischemic stroke in a different vascular territory at 90 days, compared to only 1 of 267 patients in the control arm.
More from this author: Meta-analysis suggests endovascular therapy improves stroke outcomes, Magnetic resonance imaging may aid detection of pulmonary hypertension, Breast ultrasound may improve cancer detection in dense breasts, Optical molecular imaging improves lesion localization during liver procedures, Embolization effective for treatment of upper GI bleeding in unstable patients
Image: CC/Wiki/Blausen
©2014 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. No article should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2 Minute Medicine, Inc.