#VisualAbstract: Ipatasertib plus abiraterone improves survival in PTEN-negative prostate cancer patients compared to abiraterone alone
1. Ipatasertib-abiraterone treatment significantly improved progression-free survival compared to placebo-abiraterone in patients with PTEN-loss metastatic castration-resistant prostate cancer.
2. Grade 3 or greater adverse events occurred in 70% of patients treated with ipatasertib plus abiraterone versus 39% in placebo plus abiraterone.
Evidence Rating Level: 1 (Excellent)
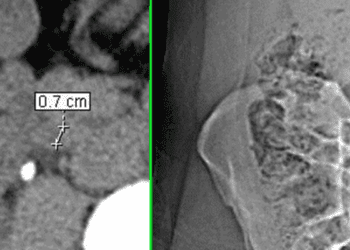
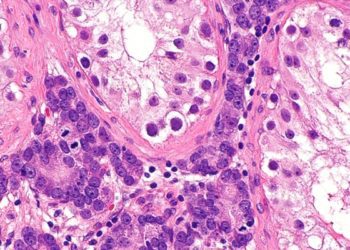
Study Rundown: Metastatic castration-resistant prostate cancer (mCRPC) is currently treated with abiraterone, an androgen biosynthesis inhibitor. Despite being an effective androgen-deprivation therapy, the median life expectancy for mCRPC is less than 3 years as patients go on to develop treatment-resistant disease. Activation of the P13K/AKT pathway is one mechanism of abiraterone resistance, which is especially hyperactive in tumors with PTEN-loss. PTEN is a tumor suppressor which is lost in approximately half of patients with mCRPC. Ipatasertib is an inhibitor of the PI3K/AKT pathway and has been shown in previous studies to have a greater effect in those patients with PTEN-loss. For these reasons, this multicenter randomized-control trial assessed the effect of dual ipatasertib-abiraterone treatment compared to placebo-abiraterone in patients with mCRPC. The 1101 enrolled patients were randomized 1:1 and stratified by PTEN-loss status. After a median follow-up of 19 months, radiographical progression-free survival was calculated. Results for the PTEN-loss group showed ipatasertib plus abiraterone significantly increased median progression-free survival compared to abiraterone alone. These numbers were similar in the intention-to-treat group, but not statistically significant. Drug adverse events were comparable to those seen in other ipatasertib trials, with the most common being a rash. Side effects that led to treatment discontinuation occurred in 5% and 21% of patients in the abiraterone only and ipatasertib plus abiraterone groups, respectively. A limitation of this study was that PTEN-loss status was archival and not updated at the time of the study. Since many tumors progress to lose PTEN, this may mean that the stratification was not accurate. Nonetheless, this study provides support for the combination of abiraterone and ipatasertib for mCRPC in patients with PTEN-loss, which usually demarcates more severe disease.
Click to read the study in the Lancet
In-Depth [randomized controlled trial]: This randomized, double-blind, phase 3 drug trial enrolled 1101 patients from 200 sites across 26 countries or regions. The eligibility criteria included 18+ years of age, mCRPC, ECOG of 0 or 1 and status defined as untreated asymptomatic or mildly symptomatic. Patients were randomized to receive placebo-abiraterone 1000 mg (n=554) once daily or ipatasertib 400mg-abiraterone 1000mg (n=554) once daily. All patients received 5 mg of prednisolone twice daily. Patients were stratified based on previous treatment and PTEN-loss status confirmed by an archival or current immunohistochemistry result. Recruitment started on June 2017 with data cut-off in March 2020. For the results, patients were analyzed as part of the PTEN-loss group (n=261 placebo, n=260 ipatasertib) or intention-to-treat (all patients). For PTEN-loss patients, progression-free survival was longer in the ipatasertib group (18.5 months) than the placebo group (16.5 months; HR 0.77, p=0.034, significant at ɑ=0.04). This trend was also seen in the intention-to-treat group (HR 0.84, p=0.043, ɑ=0.01), but the result was not significant. In terms of adverse events, grade 3 or higher events were seen in 39% of patients treated with placebo compared to 70% treated with ipatasertib. Treatment-related deaths were two in each group.
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.