Isolation of Clostridium difficile-carriers linked to lower hospital transmission
1. Screening for and isolating carriers of Clostridium difficile at admission to hospital was associated with lower rates of healthcare-associated C. difficile infection (HA-CDI) at a single institution in Quebec, CA.
2. A multi-center study would be needed to identify the effectiveness of this strategy in a broader population.
Evidence Rating Level: 2 (Good)
Study Rundown: Infection with C. difficile, a common healthcare associated infection that can result in prolonged hospital stays, readmissions, morbidity and mortality, is an important health care issue. Spore transmission can occur while in hospital to other patients. Currently, measures to decrease HA-CDI are aimed at isolating symptomatic patients with diarrhea. The current study was a quasi-experimental intervention designed to screen for and isolate asymptomatic C. difficile carriers at admission to potentially prevent the rates of HA-CDI.
The results of the study showed that, over time, screening for and isolating C. difficile carriers at admission reduced the rates of HA-CDI. At 17-month follow-up, it was estimated that two-thirds of the HA-CDI cases were prevented with a number needed to screen of 121 to prevent one HA-CDI case. While the quasi-experimental nature of the study did make the results valid, a single institution study prevented generalizability. Furthermore, clinician practices changed during the study implementation, namely antibiotic use, hand hygiene, and proton pump inhibitor use, which confounded the results.
Click to read the study, published today in JAMA Internal Medicine
Relevant Reading: Pathway to Prevention of Nosocomial Clostridium difficile Infection
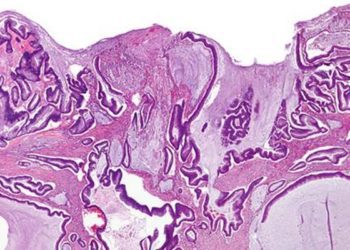
In-Depth [quasi-experimental controlled study]: This study was performed at the Quebec Heart and Lung Institute. The study evaluated rates of HA-CDI before and after implementation of the screening and isolation program in four-week periods from August 22, 2004 to March 7, 2015, with the intervention starting on November 19, 2013. Other hospitals in the province were used as controls to account for larger, systematic changes that may have taken place surrounding this issue. Diagnosis of CDI was based on the presence of diarrhea, plus one of positive assay for C. difficile, colonoscopy findings of pseudomembranous colitis, or histopathologic diagnosis. CDI was considered healthcare-associated if it occurred 72 hours after admission and up to 4 weeks after discharge. The intervention consisted of screening asymptomatic patients on admission with PCR detection of the tcdB gene on anal swab. Patients who were positive were placed under infection control measures.
Screening occurred in 92.5% of eligible patients and 4.8% of those screened were positive for carrier status and isolated. Rates of HA-CDI for 4-week periods following the intervention initially did not change (p=0.92) but then decreased at a rate of 7% per 4 week period (RR 0.93, 95% CI 0.87-0.99 per 4-week period). HA-CDI rates in the control group increased during the same period. Rates of community- and ambulatory care-acquired CDI remain unchanged. Rates of antimicrobial (RR 1.004; P<0.001) and proton pump inhibitor use increased slightly (RR 1.005; P<0.001) during the study period. Hand hygiene compliance increased from 36.6% to 49.7% (p<0.001) during the study period. The proportion of the epidemic associated NAP1 strain of C. difficile decreased from 59.2% to 20.0% (p=0.049) following the intervention.
Image: PD
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.