Laparoscopic staging may detect more advanced cervical cancer
1. After clinical staging, one-third of cervical cancer patients were upstaged (found to have nodal or peritoneal spread) on laparoscopy.
2. Laparoscopic staging of advanced cervical cancer had low rates of complications and did not significantly delay initiation of chemoradiation.
Evidence Rating Level: 1 (Excellent)
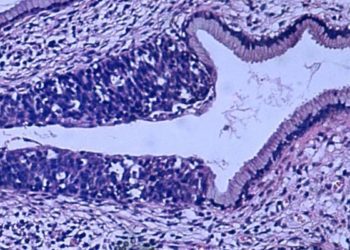
Study Rundown: While the incidence of cervical cancer and related mortality in the developed world greatly declined after the advent of the Pap smear, cervical cancer remains the third most common gynecological cancer in the United States. Infection with high-risk human papillomavirus (HPV), types 16 and 18, is central to the development of cervical cancer. Disease is classified as locally advanced when the tumor is either bulky, defined as confined to the cervix and is >4cm; invades beyond the uterus but not to the pelvic wall or lower third of the vagina; extends to the pelvic wall, involves the lower third of the vagina and/or impairs kidney function; or invades the bladder or rectal mucosa or beyond the pelvis. While lymph node metastasis is the most important prognostic factor, current guidelines recommend clinical staging which does not allow for detection of nodal involvement. Even when imaging is performed, modalities like PET-CT have limited sensitivity and specificity. Further, previous investigations demonstrate significant rates of upstaging, or confirmation of more advanced disease, when clinical staging precedes surgery. In the present work, authors evaluated the feasibility and utility of laparoscopic staging and achieved greater detection of advanced disease with minimal complications or impact on the timing of subsequent treatment.
Strengths of the study include randomized trial design. Limitations include differences in tumor grade distribution between groups and limited follow-up. Additionally, the impact on survival, which is the key outcome of interest driving this research, was not assessed. Further randomized trials evaluating long-term outcomes including disease-free and overall survival are merited to determine the clinical utility of surgical staging.
Click to read the study in AJOG
Relevant Reading: Laparoscopic staging compared with imaging techniques in the staging of advanced cervical cancer
In-Depth [randomized controlled trial]: This randomized controlled trial evaluated the impact of surgical staging of locally advanced cervical cancer (FIGO stages IIB to IVA) in women undergoing clinical and surgical staging (n=130) compared to those undergoing clinical staging alone (n=125) prior to chemoradiation therapy. Clinical staging included abdominal CT and/or MRI and/or PET-CT plus chest imaging. Both treatment arms received subsequent chemoradiation. The primary outcomes of interest were upstaging and complications. Upstaging was defined as diagnosis of a more advanced stage of cervical cancer on surgical staging.
Upstaging occurred in 33% of patients undergoing surgical staging (CI 25-42%). The rate of complications was 1.6% (CI 0.2-5.8%) intra-operatively and 7.3% post-operatively (CI 3.4-13.4%). Mean time between surgical staging and initiation of chemoradiation was 13 days.
Image: CC/Wikimedia Commons/ignis
©2015 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.