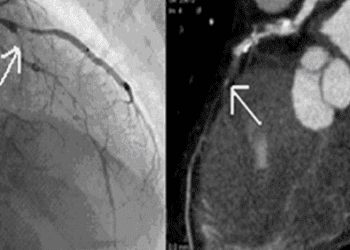
Liver fibrosis in post-PCI patients associated with higher incidence of cardiovascular events
1. Post-PCI patients with intermediate to high liver fibrosis scores were observed to experience higher incidences of major cardiovascular events.
Evidence Rating Level: 1 (Excellent)
While the introduction of percutaneous coronary interventions (PCI) have significantly reduced the rate of major cardiovascular events in patients with coronary artery disease, patients post-PCI continue to have a high risk for recurrent events and cardiovascular-related mortality. There is growing evidence that in both patients with non-alcoholic fatty liver disease (NAFLD) and the general population, the degree of liver fibrosis is a strong predictor for cardiovascular risk, of disease, events, as well as related and all-cause mortality. Although the gold standard for diagnosis of liver fibrosis is a liver biopsy, this study investigated whether noninvasive scoring systems may be a safe and accessible screening tool to predict long-term cardiovascular outcomes, particularly in patients without symptoms of or history of liver disease. In this multicentre, prospective study, 4003 patients (mean age 56.8+ 10.5 years, 76.5% male) with stable coronary artery disease undergoing PCI were assessed by eight current liver fibrosis scores (LFS) at baseline, before being followed for an average of 5.0 + 1.6 years. At 6month intervals, patients would be interviewed to assess for incidence of the primary endpoint, a composite of cardiovascular-related death, non-fatal myocardial infarction, and ischemic stroke, as well as the secondary endpoint, which included the composite primary endpoint in addition to unplanned revascularization and hospitalized unstable angina. Patients with confirmed diagnosis of liver disease and/or excessive alcohol consumption were excluded. 315 major cardiovascular events and 83 cardiovascular-related deaths were reported. Those who developed these cardiac events were more likely to have intermediate or high LFSs, based on NAFLD fibrosis score, fibrosis-4 score, BMI, AST/ALT ratio, and diabetes melitus score (BARD). Patients with intermediate to high score levels were at a significantly elevated risk, by 1.57-1.92 fold, of experiencing cardiovascular events included in the primary endpoint over patients with low LFSs. 1-SD increment on the NAFLD fibrosis score, fibrosis-4 score, AST/ALT ratio, or the BARD was associated with a 7%-59% increased risk of experiencing cardiovascular events, even after adjusting for sex, age, cardiovascular-related comorbidities, and diabetes. Adding NAFLD fibrosis score, fibrosis-4 score, and BARD to a model of established cardiovascular risk factors improved its predictability of the primary endpoint; only the NAFLD fibrosis score was independently associated with the risk of secondary endpoint events. Continued follow-up on liver fibrosis scores after baseline and conducting liver biopsies to find any unrecognized liver diseases may strengthen the results. Nonetheless, these findings support liver fibrosis scores as non-invasive, novel tools to identify high-risk patients post-PCI and aid clinical decision-making in cardiovascular risk prevention.
Click to read the study in JAHA
Image: PD
©2020 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.