Magnetic resonance imaging provides important information regarding infarct topography in determining stroke mechanism and risk
1. Magnetic resonance imaging (MRI) imaging in minor ischemic stroke patients reclassifies some cryptogenic stroke patients to small vessel occlusions.
2. Patients with MRI-defined cryptogenic embolic pattern are at a high risk of recurrent events.
Evidence Rating Level: 2 (Good)
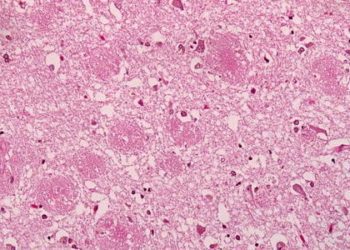
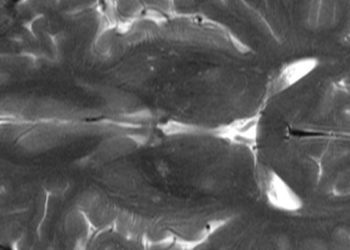
Study Rundown: Evaluating the risk of recurrence in stroke subtypes can guide secondary prevention, future investigations, and treatment thereby improving patient outcomes. A key component of this is to identify stroke etiology from the topographic presentation. To assess the relationship between the etiology, clinical pattern, and recurrence, a retrospective analysis of the dabigatran treatment of acute stroke II (DATAS II) trial was done. This included 305 adult patients with minor ischemic stroke. Of these patients, 148 had embolic pattern infarcts, 93 were isolated small subcortical infarcts and 64 had no infarct on baseline magnetic resonance imaging (MRI). When including diffusion-weighted imaging (DWI) imaging to clinical classifications, 7.9% of cryptogenic strokes were reclassified to small vessel occlusion strokes. The relative risk increase of recurrent infarction for cryptogenic strokes was increased compared to other categories standardized coefficient=1.0 (0.1, 1.9), p=0.029). Overall, study findings demonstrate that for 7.9% of cases, definitive identification of infarct topography in minor ischemic stroke/TIA caused a change in the etiology subtype. This change was most commonly going from an unknown etiology to a small-vessel occlusion, but the opposite was also seen. When DWI imaging is used in topographic characterization of infarcts, cases were often reclassified as small subcortical infarcts from a cryptogenic classification of stroke. Additionally, patients with MRI-defined cryptogenic embolic pattern are at a high risk of recurrent events.
Click to read the study in Neurology
Relevant Reading:
Dabigatran Treatment of Acute Noncardioembolic Ischemic Stroke
In-Depth [retrospective analysis of randomized controlled trial]: In patients with embolic stroke of unknown source (ESUS), the rate of recurrence is high and thought to be due to a persisting source of embolization. Recently completed ESUS trials showed that prophylactic anticoagulant therapy with rivaroxaban or dabigatran, the recurrence rate was not in patients with embolic pattern of infarction. The failure of these trials to show a benefit of anticoagulation suggests another mechanism for the increased recurrence rate. If a mechanism is identified, secondary prevention, investigations, and treatment of ESUS will be improved leading to improved patient outcomes. Many trials in the past have aimed to develop classification systems to help identify the infarct mechanism for this reason. The diagnostic criteria used in these studies vary. In this study, data from the dabigatran treatment of acute stroke II (DATASII) trial was used. The DATASII trial randomized patients to dabigatran or asprin within 72 hours of onset regardless of infarct pattern and stroke risk factor workup. This study aimed to determine the impact of MRI-defined infarct pattern on the etiological classification and recurrent infarction rate in patients with lacunar versus embolic infarcts.
Patients with non-cardioembolic minor stroke or transient ischemic attack (TIA) with (National Institutes of Health Stroke Scale (NIHSS) score≤9, infarct volume ≤25mL) were recruited and randomized to dabigatran or aspirin within 72 hours of onset. An MRI was performed before randomization and on day 30 to look at infarct volume and location. The stroke mechanism was decided using a previously described criteria (TOAST) and a consensus definition of ESUS by a blinded investigator. ‘Large-artery atherosclerosis’ mechanisms were determined by ≥50% stenosis of an extracranial or intracranial artery supplying the territory of the baseline infarct. “Cardioembolism” mechanisms were classified based on risk factors such as bioprosthetic cardiac valve, recent myocardial infarction, patent foramen ovale, and congestive heart failure. Finally, patients that did not fall into either category, lacked cortical symptoms, and had an isolated small subcortical infarct pattern on DWI were classified as “small-vessel occlusion.”
Of the 305 total patients, 148 patients showed an embolic pattern, 93 showed isolated small subcortical infarcts, and 64 had no infarct on baseline MRI. Based on the TOAST stroke mechanism classification, 48.3% of patients had stroke of unknown etiology and 40.3% of patients had small-vessel occlusion. When DWI analysis was added, most patients were found to have congruous clinical and MRI findings. 19 (6.2%) patients originally classified as unknown etiolgy stroke by TOAST criteria, were re-classified as ‘small-vessel occlusion’ based on solitary subcortical infarct topography. 5.7% of patients with isolated subcortical infarcts had cortical clinical findings.
On repeat MRI 30 days post-event, new lesions were detected in 23 patients (22 on DWI, 1 on T2). 73.9% of these lesions were not clinically identified as a stroke. 4 patients had stroke symptoms on day 30 but no new lesion on imaging. 16 of these 27 patients had an undetermined etiology at baseline showing an increased relative risk (standardized coefficient=1.0 (0.1, 1.9), p=0.029).
Image: PD
©2025 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.