Magnetic resonance imaging-targeted biopsy noninferior to standard biopsy for prostate cancer screening
1. Magnetic resonance imaging with targeted and standard biopsy was non-inferior for the detection of clinically significant cancers compared to standard biopsy only.
2. The detection of clinically insignificant cancers was less in the MRI group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Prostate cancer screening reduces prostate cancer mortality but has high rates of overdiagnosis of clinically insignificant prostate cancers. Magnetic resonance imaging (MRI) can visualize the suspicious lesions for biopsies and prevent biopsies where no visible lesions are seen. As such this study conducted a noninferiority trial between MRI-targeted biopsy with a standard biopsy and standard biopsy only for prostate screening. The primary outcome of non-inferiority was met where the percentage of clinically significant cancers was similar between the standard biopsy group and the MRI group. Furthermore, the MRI imaging group led to less clinically insignificant cancers biopsied compared to the standard biopsy group. The study was limited by the generalizability of the results as Sweden has a centralized radiologic and pathological assessment, which may not be the same in other healthcare systems. Nonetheless, the results from the study are significant as they demonstrated MRI-targeted and standard biopsy to be non-inferior to standard biopsy alone for prostate cancer screening.
Click here to read the study in the NEJM
Relevant Reading: Detection of Prostate Cancer Using a Multistep Approach with Prostate-specific Antigen, the Stockholm 3 Test, and Targeted Biopsies: The STHLM3 MRI Project
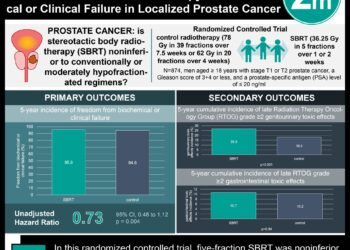
In-Depth [randomized controlled trial]: This population-screening, randomized control trial invited 12,750 men in Stockholm County, Sweden. Men between 50 to 74 years of age and a previous prostate biopsy more than 60 days before the invitation were included in the study. Patients who were previously diagnosed with prostate cancer or a previous prostate cancer biopsy within 60 days of the invitation were excluded from the study. Of the initial 12,750 men invited for the study, 1,532 men had PSA levels of 3 ng per milliliter or higher and were randomized in a 2:3 ratio of either standard biopsy (standard group) or MRI and proceeding with standard and targeted biopsies (MRI group), respectively. In the intention-to-treat analysis, clinically significant cancer was found in 21% of the experimental group compared to 18% in the standard group (difference, 3 percentage points; 95% confidence interval [CI], -1 to 7%; p < 0.001 for noninferiority). Clinically insignificant cancers were detected in 4% of the experimental arm compared to 12% in the standard arm (difference, -8 percentage points; 95% CI, -11 to -5). If the standard biopsy was ignored in the MRI group, the experimental group would have not met the non-inferiority criterion at the 2.5% alpha level. Overall, the addition of MRI with standard and targeted biopsy has the potential to discriminate against clinically irrelevant lesions; however, costs and availability of MRIs will be key factors in the implementation of a cost-effective prostate cancer screening program.
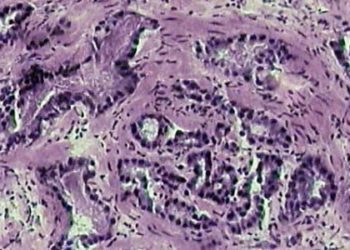
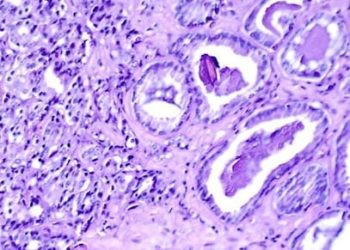
Image: PD
©2021 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.