Mild-to-moderate hypertriglyceridemia associated with higher risk of acute pancreatitis
1. This prospective cohort study, conducted in Copenhagen, found that mild-to-moderate levels of non-fasting hypertriglyceridemia, from 177 mg/dL (2 mmol/L) and above, were associated with increased risk of acute pancreatitis.
2. These increases in risk for acute pancreatitis were greater than the corresponding risk of myocardial infarction within the same triglyceride range.
Evidence Rating Level: 2 (Good)
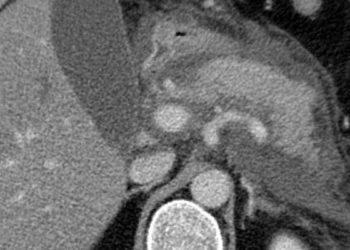
Study Rundown: It is well established that high levels (>885 mg/dL; >10 mmol/L) of plasma triglycerides is associated with acute pancreatitis, but it is unclear if this increased risk exists with mild-to-moderate elevation as well. This prospective cohort study aimed to determine if non-fasting mild-to-moderate hypertriglyceridemia (177-885 mg/dL; 2-10 mmol/L) was associated with acute pancreatitis.
Compared to individuals with triglyceride levels of <89 mg/dL (<1 mmol/L), there was a significant stepwise increase in risk of acute pancreatitis for every 89 mg/dL (1 mmol/L) increase in plasma triglyceride level. These increases in risk were greater than the risk of myocardial infarction with the same corresponding level of serum triglycerides. These results remained robust in multivariable regression when stratified for multiple potential confounders. Strengths of this study included its prospective design and using a population cohort. Limitations included inclusion of primarily Caucasian individuals of Danish descent. Additionally, there may have been misclassifications with the use of administrative diagnostic coding for cohort and outcome definitions.
Click to read the study, published in JAMA Internal Medicine
In-Depth [prospective cohort study]: This prospective cohort study was conducted using data from the Copenhagen General Population Study (2003-2015) and the Copenhagen City Heart Study (1976-1978 data was collected, follow-up examinations occurred in 1981-1983, 1991-1994, 2001-2003). Median follow-up time was 6.7 years. The exposure of interest was plasma non-fasting triglycerides and these levels were obtained from the databases listed above. The outcome of interest was occurrence of acute pancreatitis as defined by ICD-8, ICD-10 codes for acute pancreatitis. Coding for myocardial infarction was also analyzed as a positive control. Statistical analysis included hazard ratios calculated with Cox proportional regression models. These models were adjusted for age, sex and risk factors for pancreatitis (education, smoking, hypertension, statin use, study cohort, birth year).
In all, 116,550 individuals from both databases with a triglyceride measurement were included in the study cohort. Compared to individuals with serum triglyceride levels of <89 mg/dL (1 mmol/L), the multivariable adjusted hazard ratios (HRs) for acute pancreatitis were as follows: 1.6 (95% CI 1.0-2.6) for levels of 89 – 176 mg/dL (1.00 to 1.99 mmol/L), 2.3 (95%CI 1.3-4.0) for 177 – 265 mg/dL (2.00 to 2.99 mmol/L), 2.9 (95%CI 1.4-5.9) for 266 – 353 mg/dL (3.00 to 3.99 mmol/L), 3.9 (95%CI 1.5-10.0) for 354 – 442 mg/dL (4.00 to 4.99 mmol/L), 8.7 (95%CI 3.7-20.0) for ≥443 mg/dL (≥ 5.00 mmol/L). The corresponding HRs for myocardial infarction were 1.6 (95%CI 1.4-1.9), 2.2 (95%CI 1.9-2.7), 3.2 (95%CI 2.6-4.1), 2.8 (95%CI 2.0-3.9) and 3.4 (95%CI 2.4-4.7), respectively. The results remained robust through all adjustment and stratification of potential confounders. There was also no statistical evidence of interaction.
Image: CC/Wiki
©2016 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.