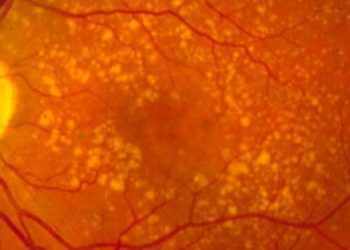
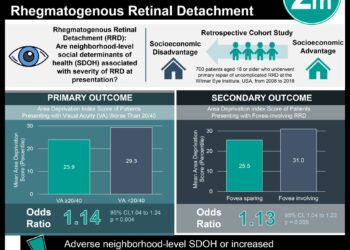
Monthly brolucizumab is noninferior to aflibercept in treating recalcitrant wet age-related macular degeneration
1. In a phase 3a randomized trial comparing intravitreal brolucizumab to aflibercept for refractory neovascular age-related macular degeneration (nAMD), there was no significant difference between drugs in visual acuity change, and brolucizumab eyes were more likely to be fluid-free at 1 year.
2. Eyes in the brolucizumab group were significantly more likely to have intraocular inflammation than eyes in the aflibercept group.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Brolucizumab is one of the newer anti-vascular endothelial growth factor (VEGF) therapies approved for treating neovascular disease of the retina, including neovascular age-related macular degeneration (nAMD). The HAWK and HARRIER trials showed brolucizumab injections every twelve weeks to be superior to other VEGF-targeting therapies such as aflibercept for visual outcomes, but also showed an increased rate of inflammatory complications. This multi-center phase 3a randomized trial, MERLIN, aimed to compare brolucizumab 6 mg to aflibercept 2 mg, both injected every 4 weeks, in the setting of retinal fluid persisting after other anti-VEGF regimens. At week 52, brolucizumab met the primary endpoint of noninferiority to aflibercept in best-corrected visual acuity (BCVA) change, with no significant difference between groups. 40.4% of eyes treated with brolucizumab were free of subretinal and intraretinal fluid at 52 weeks compared to 19.0% treated with aflibercept. However, 9.3% of brolucizumab eyes had intraocular inflammation (IOI) within the year compared to 4.5% of aflibercept eyes. The MERLIN trial was terminated due to this increase in IOI. Brolucizumab is more concentrated than aflibercept and was dosed higher here, which is consistent with both its increased efficacy by some measures here and a higher risk of harmful inflammation. This trial is the first to report on frequent dosing of brolucizumab. The risk of both inflammatory adverse events and all-causes vision loss was unacceptably high with brolucizumab dosed every 4 weeks as a long-term maintenance regimen. However, the outcomes here, particularly the substantial rate of stable fluid-free status in previously refractory eyes, point strongly to a continued role for less frequent brolucizumab in nAMD.
Click to read the study in Ophthalmology
Relevant Reading: Current and upcoming anti-VEGF therapies and dosing strategies for the treatment of neovascular AMD: A comparative review
In-Depth [randomized controlled trial]: Eyes were randomized in a 2 to 1 ratio to receive brolucizumab or aflibercept, both every 4 weeks for a planned 100 weeks. Adults aged 50 or older treated at 66 sites in the United States between 2018 and 2020 were included. Patients were required to have active nAMD with intraretinal and/or subretinal fluid and to have received at least 7 anti-VEGF injections, most frequently aflibercept, in the previous 9 months with partial but incomplete response. Patients with active IOI at baseline were excluded. The least squares mean difference in BCVA change between brolucizumab and aflibercept was -0.6 letters [95% confidence interval (CI) -2.1–0.9]. Eyes receiving brolucizumab had significantly lower central subfield thickness (CST) than aflibercept at 52 weeks. 16.9%, 22.3%, and 35.8% of patients receiving brolucizumab gained ≥15, ≥10, and ≥5 letters, respectively, compared to 17.4%, 20.2%, and 31.5% with aflibercept. 17 total eyes treated with brolucizumab lost ≥15 letters in BCVA at week 52 compared to 3 in the aflibercept group.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.