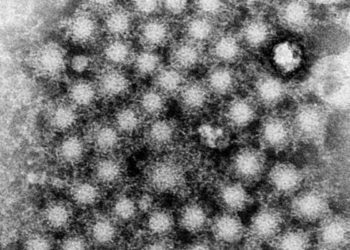
New interferon-free regimen effective in chronic HCV genotype 1 infection
Image: PD
1. Combination therapy of HCV protease inhibitor ABT-450, nonnucleoside polymerase inhibitor ABT-333, and NS5A inhibitor ABT-267 achieved high, sustained virologic response rates.
2. The new regimen had a more favorable tolerance and safety profile compared to the current gold standard.
Evidence Rating Level: 1 (Excellent)
Study Rundown: Hepatitis C viral (HCV) infection is of great public health significance due to the large number of patients impacted and the potentially disastrous disease course if left untreated, such as cirrhosis and the eventual need for liver transplant. This randomized, phase 2b trial, involving three novel anti-HCV agents, demonstrated high levels of sustained virologic response with 12 weeks of therapy and favorable safety profiles. The current standard therapy against hepatitis C of boceprevir or telaprevir still requires interferon in the “harder to treat” genotype 1 patients, a regimen with rate of discontinuation of 10% to 16% due to adverse, treatment-related events. The regimen investigated in this study resulted only in 1% discontinuation due to adverse events. This finding represents a significant advance in designing an HCV treatment regimen that is both highly effective and well-tolerated. As a phase-2 trial, the small study size has limited the power to detect between-group differences.
The study was sponsored by AbbVie.
Click to read the study, published today in NEJM
Relevant Reading: Boceprevir for previously treated chronic HCV genotype 1 infection
In-Depth [randomized controlled trial (open label, phase 2b)]: The primary goal of this phase 2 clinical trial was to determine the safety and efficacy of various combinations of anti HCV agents in patients who had not received therapies previously and in those who had failed prior therapies. The agents included ABT-450/r (HCV NS3/4A protease inhibitor ABT-450 coadministered with ritonavir), ABT-333 (nonnucleoside NS5B polymerase inhibitor), and ABT-267 (NS5A inhibitor). The primary end point was sustained virologic response (HCV RNA level under 25 IU/mL) at 24 weeks after treatment.
The rates of sustained virologic response at 24 weeks after treatment across all subgroups ranged from 83% to 100%. Among previously untreated patients, the combination of all 3 agents plus ribavirin, the sustained virologic response at 24 weeks was 88% in the subgroup that received 8 weeks of therapy and 95% in the subgroup that received 12 weeks of therapy.
Across different regimens, ABT-450/r administered as either 100 mg of ABT-450 or 150 mg of ABT-450 plus 100 mg of ritonavir had similar rates of sustained virologic response (93.6% vs. 94.3%, P=0.91). The sustained virologic response rate after 12 weeks of treatment with all three direct-acting agents plus ribavirin was 96% for previously untreated patients and 93% for those who had not had a response to prior therapy.
Across different durations of therapy using all 3 agents plus ribavirin, a 12-week therapy resulted in a higher – but not statistically significant – rate of sustained virological response compared to the 8-week therapy (96% vs 88%). A 24-week therapy did not result in a higher sustained virologic response rate compared to the 12-week treatment.
In safety analysis, a total of 8 patients (1%) discontinued the study due to adverse events. Common adverse events (> 20% of patients) included fatigue, headache, nausea and insomnia. Other less common adverse events included elevation of bilirubin, aminotransferase, and anemia.
By Xiaozhou Liu and Xu Gao
More from this author: Nivolumab plus ipilimumab shows promise for metastatic melanoma, Prophylactic platelet transfusions prevent bleeding in hematologic cancers, Azithromycin is not associated with increased cardiovascular death in low-risk groups, Health education module reduces parasitic infections, New chemotherapy precludes the need for radiotherapy in primary mediastinal B-cell lymphoma
©2012-2014 2minutemedicine.com. All rights reserved. No works may be reproduced without expressed written consent from 2minutemedicine.com. Disclaimer: We present factual information directly from peer reviewed medical journals. No post should be construed as medical advice and is not intended as such by the authors, editors, staff or by 2minutemedicine.com. PLEASE SEE A HEALTHCARE PROVIDER IN YOUR AREA IF YOU SEEK MEDICAL ADVICE OF ANY SORT.