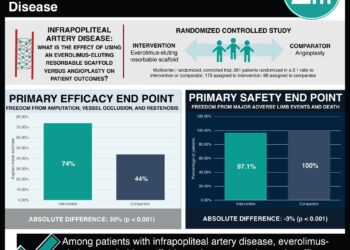
No observed benefit of adjuvant everolimus combined with endocrine therapy for hormone receptor-positive, human epidermal growth factor receptor 2 (HER2)-negative breast cancer
1. Disease-free survival did not differ significantly between patient groups and overall survival at 3 years was the same for both groups.
2. A higher percentage of patients receiving everolimus experienced grade 3 or worse adverse effects as compared to those receiving placebo.
Evidence Rating Level: 1 (Excellent)
Study Rundown: In the first 10 years after treatment with endocrine therapy (ET), roughly 20% of patients with hormone receptor-positive, human epidermal growth factor receptor 2 (HER2)-negative breast cancer have disease recurrence. Resistance to ET is via a dysregulation of the phosphatidylinositol-3-kinase/Akt/mammalian target of rapamycin (mTOR) pathway. Everolimus is an mTOR inhibitor, and its combination with ET has showed prolonged progression-free survival (PFS) in both advanced and metastatic hormone receptor-positive HER2-negative breast cancer. This study aimed to compare the outcomes on disease-free survival (DFS), overall survival (OS), and safety of everolimus with ET to placebo with ET in women who were hormone positive breast cancer, HER2 negative in the adjuvant setting. The overall 3-year DFS was not statistical different in the overall group and in the subgroups with tamoxifen or aromatase inhibitor (AI). There was no difference in OS at 3 years. The most common grade 3 or 4 AEs were oral mucositis, hypertriglyceridemia, elevated liver enzymes, fatigue, and hyperglycemia. A higher percentage of patients in the everolimus group experienced these AEs, compared to those in the placebo group. Treatment withdrawal due to AEs occurred in 35.3% of patients in the everolimus group as compared to 10.0% of those on placebo. There was one death due to everolimus treatment. Limitations to this study include the inclusion of both premenopausal and menopausal patients as the different biology between these patients may have introduced a confounding component to the analysis of ET subgroups. Overall, the use of everolimus in the adjuvant setting for treatment of hormone receptor-positive, human epidermal growth factor receptor 2 (HER2)-negative breast cancer cannot be recommended.
Click to read the study in The Journal of Clinical Oncology
Relevant Reading: Everolimus in postmenopausal hormone-receptor–positive advanced breast cancer
In-Depth [randomized controlled trial]: This double-blind, international, multi-centre study randomly assigned 1,278 adult female patients in a 1:1 ratio to receive either everolimus (637 patients) or placebo (641 patients) in combination with ET treatment for 2 years. The patients were further stratified by the type of ET aromatase inhibitors (AIs) versus tamoxifen ± luteinizing hormone-releasing hormone agonists. Initially, 10mg of everolimus daily was provided as a starting dose, but due to toxicity was decreased to 5mg with flexibility to increase to 10mg. The overall 3-year DFS did not differ and was 88% (95% confidence interval (CI), 85-91%) for the everolimus group and 89% (95% CI, 86-91%) for the placebo group (hazard ratio (HR) = 0.95; 95% CI, 0.69-1.32). The DFS for patients on AI was 87% (95% CI, 82-90%) in the everolimus group and 91% (95% CI, 87-93%) in the placebo group (HR = 1.25, 95% CI, 0.83-1.90). For patients on tamoxifen treatment, DFS was 91% (95% CI, 86-94%) in the everolimus group and 86% (95% CI, 81-90%) in the placebo group (HR = 0.62, 95% CI, 0.37-1.06). There was no difference in OS at 3 years and both groups had 96% (95% CI, 94-98% for everolimus, and 95%CI, 94-97% for placebo). The hazard ratio was 1.09 (95% CI, 0.62-1.92). The majority of patients in each group had experienced an AE (98.1% of those on everolimus, and 96.5% of those on placebo) and the most common grade 3 or 4 AEs were mucositis, hypertriglyceridemia, elevated liver enzymes, fatigue, and hyperglycemia; these were all higher in the everolimus treatment group. Serious AEs occurred in 11.8% of those on everolimus, and 9.3% of those on placebo; 38.2% of patients on 10mg of everolimus experienced AEs grade 3 or worse compared to 15% of patients on placebo and 25.4% of patients on 5mg of everolimus had AEs grade 3 or worse, compared to 16.1% of those on placebo. Treatment withdrawal occurred in 35.3% of those in the everolimus groups and 10.0% of those in the placebo groups. One patient died secondary to everolimus treatment.
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.