Patient Basics: Cervical Cancer
Originally published by Harvard Health.
What Is It?
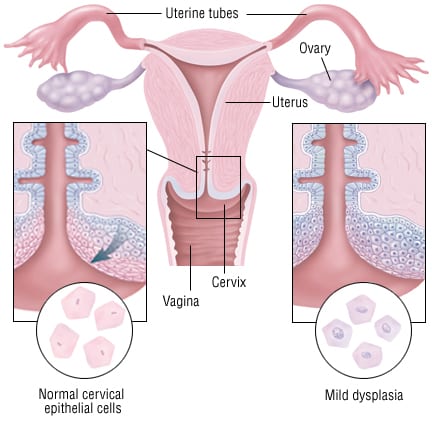
The cervix is a small, donut-shaped structure. It is located at the top of the vagina. It is the entrance to the uterus.
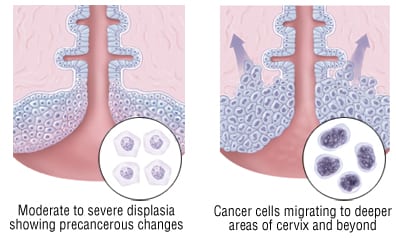
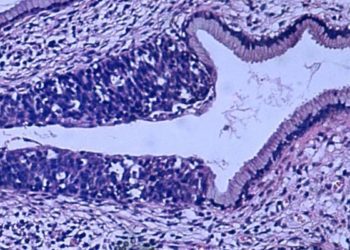
Cervical cancer begins in the outer layer of the cervix. This outer layer is called the cervical epithelium. Tiny changes begin in epithelial cells. Over time, cells may become cancerous and grow out of control.
Cervical cancer usually grows slowly. It can remain in the cervical covering for up to 10 years. Once cervical cancer moves beyond this layer, it invades nearby tissue. This includes the uterus, vagina, bladder, and rectum.
Almost all cervical cancer is caused by infection with human papilloma virus (HPV). HPV can damage the cells that line the cervix. Sometimes the damage occurs in the genes of the cells, which may lead to cervical cancer.
HPV is a very common infection among sexually active women. But only a small number of women with HPV develop cervical cancer.
Smokers are more likely to develop cervical abnormalities if they are infected with HPV. Women infected with human immunodeficiency virus (HIV) are also at higher risk.
Symptoms
In its early stages, cervical cancer does not cause any symptoms. When cervical cancer does cause symptoms, a woman may experience:
- Blood-tinged or discolored vaginal discharge
- Spotting after sex
- Heavier and/or more prolonged menstrual bleeding
- Vaginal bleeding between periods
These symptoms do not mean that you have cervical cancer. In fact, a woman may experience these symptoms for many reasons.
More advanced cervical cancer can cause:
- Pelvic pain
- Loss of appetite
- Weight loss
- A decrease in red blood cells (anemia)
Diagnosis
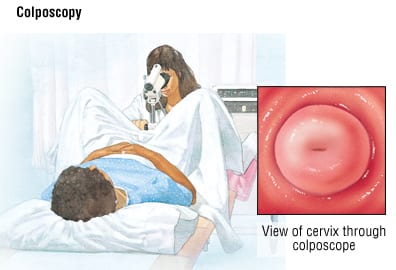
Diagnosis of cervical cancer usually begins with a pelvic exam. The doctor inspects your cervix and vagina. He or she performs a Pap test. During a Pap test the doctor obtains a sample of cells from the surface and canal of your cervix. The cells are sent to a laboratory for examination. The Pap test is a quick, painless procedure.
If the Pap test indicates abnormal or possibly cancerous cells, a gynecologist will do one or more of the following:
- Examine your cervix and vagina with a magnifying instrument.
- Perform a biopsy. Your doctor removes a small piece of tissue from the cervix to be examined in a laboratory.
- Take a scraping of the cells inside the inner opening of the cervix.
- Perform a DNA test to check for HPV infection.
DNA testing can also identify the type of HPV. This is important because some types of HPV are more likely than others to cause cancer.
Your HPV DNA test may suggest a higher risk of developing cancer. If that is the case, your doctor may recommend further testing be done soon. Women who have a lower risk may be able to wait a few months before having a follow-up Pap smear.
Expected Duration
Cervical cancer grows slowly and can take years to invade nearby tissues. However, it will continue to grow until it is treated.
Prevention
Almost all cervical cancer is caused by infection with HPV. There are currently two available HPV vaccines that target the major cervical cancer-causing types of HPV. The vaccines do not protect against all types of HPV.
The Centers for Disease Control and Prevention (CDC) recommends that all females starting at ages 11 or 12 get the HPV vaccine. Older girls and young women up to age 26 also should be vaccinated. Girls as young as nine years old may receive the vaccine. The vaccine is given as a set of three shots over six months.
Detecting cervical cancer early dramatically increases your chances of a cure. That is why Pap tests are an important part of prevention.
Women at average risk of cervical cancer should begin regular Pap testing at age 21. Pap smears should be done once every 3 years until age 30, as long as prior Pap smears have been normal. No HPV screening for women under age 30.
Women age 30 and over can be screened with a Pap smear once every three years if they have had three normal Pap smears in a row. If a women age 30 or older has HPV testing and the HPV test is negative, Pap smears can be done once every 5 years.
Women that have an increased risk of cervical cancer need more frequent screening. Usually this means at least once per year. Risk factors that increase risk include:
- HIV infection
- Conditions or medications that decrease immunity
- Having a mother that took the drug diethylstilbestrol (DES) during pregnancy
- Any prior cervical biopsies that showed cancerous cells
Other steps to help prevent cervical cancer:
- Limit your number of sexual partners to reduce possible exposure to HPV.
- Use condoms during vaginal sex (unless you have only one sexual partner who you know does not have any sexually transmitted diseases).
- If you smoke, quit.
Treatment
The cancer’s stage is determined by how far the cancer has spread. Treatment depends on the stage.
- Stage 0 cancer remains within the surface layer.
- Stage I cancer remains within the cervix.
- Stage II cancer extends beyond the cervix, but not to the pelvic wall or into the lower portion of the vagina.
- Stage III cancer extends into the pelvic wall, the lower portion of the vagina or the tubes that connect the kidneys to the bladder.
- Stage IV cancer extends beyond the pelvis or involves the bladder, the rectum or both.
When recommending treatments for Stage 0 or Stage I cancer, your doctor will consider whether you want to have children. A pregnant woman diagnosed with Stage 0 or Stage I cervical cancer may be able to postpone treatment until after birth.
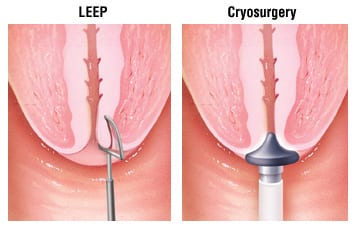
A woman with Stage 0 cancer who still wants to have children is usually treated with a surgical procedure to do one of the following:
- Heat and vaporize the surface tissue layer
- Freeze epithelial tissue to destroy abnormal cells
- Surgically remove a cone-shaped piece of cervical tissue
- Remove abnormal cells from the cervix using an electric current
For two years after these procedures, women should have frequent Pap tests to check for abnormal cells.
In women with Stage I cancer that plan to become pregnant, doctors may remove a cone-shaped piece of cervical tissue. For women who don’t plan to become pregnant, the treatment for a minimally invasive Stage I cancer is usually a total hysterectomy. A total hysterectomy is the removal of the uterus and cervix.
Larger Stage I and Stage II cancers require a radical hysterectomy or radiation therapy plus chemotherapy. A radical hysterectomy is the removal of the uterus, cervix, ovaries, fallopian tubes and pelvic lymph nodes. The choice between surgery and radiation therapy partly depends on the woman’s age and health. The doctor should also consider the patient’s concerns about potential side effects or complications.
The mainstay of treatment for Stage III and Stage IV is radiation. Combining chemotherapy with radiation therapy helps to improve survival in these later stages.
When to Call a Doctor
Report any of the following symptoms to your doctor:
- Abdominal pain
- Weight loss
- Unusual discharge from the vagina
- Blood spots or light bleeding outside the time of your normal period
- Significant pain or bleeding during sex
Remember that these symptoms don’t necessarily mean that you have cancer.
For women with advanced cervical cancer, significant vaginal bleeding requires immediate medical attention.
Prognosis
Survival depends on the stage at which the cancer is discovered and treated. Almost 100% of women with Stage 0 disease are cured. Women with Stage 1 and Stage 2 disease have a very good chance for cure. Cure rate is substantially lower if cervical cancer is discovered at a later stage.
Additional Info
National Cancer Institute (NCI)
Public Inquiries Office
Suite 3036A
6116 Executive Blvd., MSC 8322
Bethesda, MD 20892-8322
Toll-Free: 1-800-422-6237
TTY: 1-800-332-8615
http://www.nci.nih.gov/
American Cancer Society (ACS)
1599 Clifton Rd., NE
Atlanta, GA 30329-4251
Toll-Free: 1-800-228-2345
TTY: 1-866-228-4327
http://www.cancer.org/
Cancer Research Institute
One Exchange Plaza
55 Broadway
Suite 1802
New York, NY 10022-4209
Toll-Free: 1-800-992-2623
Fax: 212-832-9376
http://www.cancerresearch.org/