Patient Basics: Herniated Disk
Originally published by Harvard Health.
What Is It?
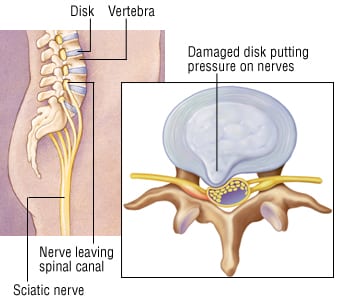
The disks in your spine, called intervertebral disks, are thin, oblong structures that serve as cushions between the bones of your back (vertebrae). Each disk is made of a soft gel core surrounded by a tough, fibrous outer shell. This structure allows the disk to be firm enough to maintain the space between the vertebrae, but soft enough to compress when the spine flexes during bending, leaning and turning sideways.
In some people, mostly middle-aged adults, a disk’s tough outer shell develops an area of weakness or a small tear. When this happens, part of the disk’s soft inner core can bulge out of its normal position (herniate), producing a condition called a herniated disk. If the herniated disk presses on nerves in the nearby spinal canal, this can cause variety of nerve-related symptoms, including pain, numbness and muscle weakness. In the most severe cases, a herniated disk can compress nerves that control the bowel and bladder, causing urinary incontinence and loss of bowel control.
Scientists do not fully understand why disks herniate. Most theories attribute this condition to a combination of the following factors:
- Disk aging – Herniated disks are rare in young people, but common among people aged 35 to 55. Of all the factors responsible for herniated disks, aging is probably the most important. With age, the disk’s outer shell appears to degenerate slowly, possibly because of decades of upright posture and back flexion.
- Genetic factors – In some families, several close relatives suffer from herniated disks, whereas other families are not affected at all. If the condition runs in a family, it may have an unusually early onset, even striking people younger than 21. Studies are beginning to identify specific genes linked to inherited forms of disk disease.
- Individual risk factors – You may be at increased risk of a herniated disk if you work at a job or participate in a sport that involves heavy lifting or excessive twisting or bending.
There are three distinct areas of the vertebral column where a herniated disk may occur:
- The cervical area between the vertebrae in the neck
- The thoracic area between the vertebrae in the upper back, near the ribs
- The lumbar region between the vertebrae in the lower back, above the pelvis
Herniated disks are most common in the lumbar region. Herniated disks are relatively rare in the thoracic region, where they account for only 1 in every 200 to 400 disk herniations.
Symptoms
The first symptom of a herniated disk is usually back pain in the area of the affected disk. Some researchers believe this pain is a signal that a disk’s tough outer shell has been injured or weakened, not necessarily that the inner core has herniated. If the inner core does herniate and press on a nearby nerve, the resulting symptoms vary depending on the location of the herniated disk:
- In the cervical region – There can be pain in the neck, shoulder, shoulder blade, arm or chest, together with numbness or weakness in the arm or fingers. If the pain is centered in the chest and arm, it can mimic the chest pain of heart disease. Occasionally, frequent urination and headaches can occur.
- In the thoracic region – Symptoms tend to be vague, misleading and long lasting. There may be pain in the upper back, lower back, chest, abdomen or legs, together with weakness and numbness in one or both legs. Some affected people also complain of bowel or bladder incontinence.
- In the lumbar region – Many people suffer from years of intermittent and mild lower back pain before a single triggering event (such as heavy lifting, sudden bending, abrupt twisting) aggravates their symptoms to the point that they seek medical attention. It also may develop without an identifiable triggering event. In most people with a lumbar disk herniation, severe leg pain is the chief complaint. This pain is called sciatica because it comes from pressure on the sciatic nerve. It usually begins in the lower back, then spreads into the buttocks and down the back of one thigh and leg. Sciatica typically becomes worse if the patient coughs, sneezes, bears down or moves the back abruptly. While often relieved by rest, sciatica may become worse with driving or lifting. In addition, there may be numbness, tingling or muscle weakness in the buttocks or leg on the side of the pain. In rarer and more severe forms of lumbar disk herniation, the nerve is compressed more extensively. If this happens, additional symptoms can develop, including rectal pain; loss of bowel and bladder control; and numbness around the genital area, buttocks or backs of the thighs.
Diagnosis
Your health care professional will review your medical history, including any history of fever, cancer, steroid use or recent back injuries. Your doctor then will ask you specific questions about your pain:
- Have you had milder episodes of back pain in the past?
- Where is your pain located? Is it limited to your back or does it spread into your shoulder, arm, chest, buttock or leg?
- When did your pain start? Did it begin when you tried to lift something heavy, or was it triggered by a sudden twist or bend of your back?
- What makes it feel better, and what makes it worse?
- Does the pain disappear when you rest the affected area, or is it present even at rest?
- Have you noticed any numbness, tingling or muscle weakness in your arms or legs?
- Are there problems with bowel or bladder control, rectal pain, or numbness in the buttocks or genital area?
After reviewing your medical history and symptoms, your doctor will do a thorough physical examination to rule out other illnesses that can cause back pain, such as cancer or a bone infection of the vertebrae.
This general physical exam will be followed by a more detailed examination of your back, during which your doctor will look for differences between your right and left sides, muscle spasms, abnormal curvature, limitation of movement, lack of flexibility, areas of numbness, and areas of tenderness. Your doctor’s findings will help to rule out other types of back problems that can cause similar symptoms.
If you have symptoms of lumbar disk herniation, your doctor may ask you to do specific maneuvers, such as walking on your toes, walking on your heels, squatting and standing, and flexing your ankle against resistance. Your doctor will want to do a straight leg-raising test. You will lie on your back with your legs straight. While you relax, your doctor slowly raises each leg individually to determine the angle where your leg pain begins. Your doctor will do a neurological examination, looking for changes in your reflexes, as well as for any evidence of muscle weakness or decreased sensation.
Spinal X-rays, a computed tomography (CT) scan or magnetic resonance imaging (MRI) scan may be recommended if your initial diagnosis is not clear, if your symptoms persist or worsen after several weeks of treatment, or if you are considering surgery. Because imaging tests, such as MRI or a CT scan, may show disk abnormalities even in people without symptoms, the results must be interpreted carefully. It is common to find abnormalities that have no effect on symptoms. Your doctor also may recommend an electromyography, a test that analyzes muscle and nerve function to identify sites of nerve compression or irritation.
Expected Duration
In most people, back pain gradually improves within four to six weeks of treatment.
Prevention
In many cases, it is not possible to prevent a herniated disk. However, if you have suffered from a herniated disk in the past, you may be able to decrease your chances of it happening again by:
- Avoiding activities that require heavy lifting or repetitive bending
- Practicing good posture
- Maintaining a healthy weight
- Following a physical-therapy program aimed at building muscle strength in your back and improving abdomen and back flexibility
- Exercising regularly, especially swimming and walking
Treatment
In most cases, a herniated disk (with or without sciatica) will respond to conservative treatment. This may include limited bed rest (generally no more than a day or two); warm baths; heating pads; and medications, such as aspirin or other nonsteroidal anti-inflammatory drugs (NSAIDs) or muscle relaxants. Some doctors prescribe oral corticosteroids, although the benefits of this treatment are uncertain.
Because prolonged inactivity can promote deconditioning, your doctor may suggest that you start an exercise regimen early. Even if you begin your treatment with one to two days of bed rest, you may still be asked to complete two or three 20-minute periods of walking each day. After one to two weeks, you usually can begin a more strenuous program of daily aerobic exercises (walking, biking, swimming) and physical therapy. Other types of conservative treatment that have been helpful to some people include ultrasound, massage and acupuncture.
When these more conservative measures don’t work, epidural steroid injections may be helpful. This involves the careful injection of a long-acting steroid and an anesthetic into the space near the spinal cord and compressed nerves. These injections are guided by X-rays or CT scanning so that the needle can be placed precisely in the proper location. If you have lost bowel or bladder control, if you have evidence of progressive nerve damage, or if you have unrelenting pain that persists despite weeks of conservative treatment, more aggressive treatment may be needed, including surgery. In most cases, this means removing the disk (diskectomy), which may require major surgery. Increasingly, though, a less invasive operation is done in which the herniated disk is removed through a hollow tube inserted through a tiny incision.
When To Call a Professional
Call your health care professional immediately if you develop severe back pain, especially if you also have pain or numbness in your arms or legs or if you lose control of your bowels or bladder.
Prognosis
About 60% of people respond to conservative therapy within 1 week, and 90% to 98% respond within 6 weeks. Surgical intervention has a high success rate when MRI or CT shows that the cause of the symptoms can be corrected.
Additional Info
National Institute of Arthritis and Musculoskeletal and Skin Diseases
Information Clearinghouse
National Insitutes of Health
1 AMS Circle
Bethesda, MD 20892-3675
Phone: 301-495-4484
Toll-Free: 877-226-4267
TTY: 301-565-2966
http://www.niams.nih.gov/
American Academy of Orthopaedic Surgeons (AAOS)
6300 North River Road
Rosemont, IL 60018-4262
Phone: 847-823-7186
http://orthoinfo.aaos.org/
North American Spine Society
7075 Veterans Blvd.
Burr Ridge, IL 60527
Toll-Free: 1-866-960-6277
http://www.spine.org/
American Physical Therapy Association
1111 North Fairfax St.
Alexandria, VA 22314-1488
Phone: 703-684-2782
Toll-Free: 1-800-999-2782
TTY: 703-683-6748
http://www.apta.org/
Arthritis Foundation
P.O. Box 7669
Atlanta, GA 30357-0669
Phone: 404-872-7100
Toll-Free: 1-800-283-7800
http://www.arthritis.org/