Patient Basics: Pneumonectomy
Originally published by Harvard Health.
What Is It?
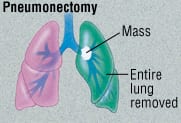
A pneumonectomy is the surgical removal of a lung.
Pneumonectomy is usually done as a treatment for cancer. It can be done in one of two ways:
Traditional pneumonectomy — Only the diseased lung is removed.
- Extrapleural pneumonectomy — The diseased lung is removed, together with:
- A portion of the membrane covering the heart (pericardium)
- Part of the diaphragm
- The membrane lining the chest cavity on the same side of the chest
Pneumonectomy removes half of a person’s breathing capacity. For this reason, surgeons usually choose a less extreme form of lung surgery if possible.
However, a pneumonectomy is probably the best option when a tumor:
- Is located in the middle of the lung
- Involves a significant portion of the pulmonary artery or veins
What It’s Used For
Most often, a traditional pneumonectomy is done to remove lung cancer. It also may be necessary when a patient has been severely wounded in the chest.
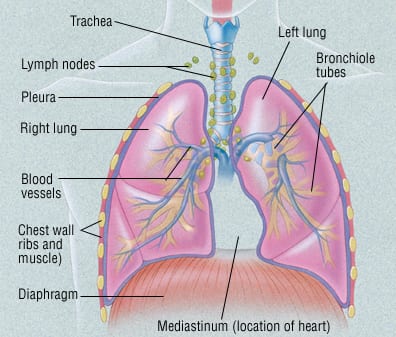
An extrapleural pneumonectomy may be a treatment option for malignant mesothelioma. This is a cancer of the pleura. The pleura is the membrane lining the chest cavity and covering the lungs. This cancer typically is caused by exposure to asbestos.
Preparation
Your doctor will order extensive testing of your lungs before a pneumonectomy. Your doctor will confirm that the remaining lung is healthy enough to take over the entire workload of breathing for your body. He or she will also make sure your heart is strong enough to withstand surgery.
Before your surgery is scheduled, you will have a series of scans and blood tests. These tests will confirm that the cancer has not spread outside your lungs. These scans may include a:
- Bone scan
- Computed tomography (CT) scan of your abdomen
- CT scan of your head
Your doctor will review your allergies and your medical history.
About one week before surgery, you will stop taking aspirin and certain anti-inflammatory medications. If you take other blood-thinning medications, check with your doctor about when to stop them.
On the night before your surgery, you must not eat or drink anything.
How It’s Done
An intravenous (IV) line will be inserted into a vein in your arm. The IV will deliver fluids and medications. You will be given general anesthesia.
An incision will be made in your chest on the side of the diseased lung. In a traditional pneumonectomy, the surgeon collapses the diseased lung and ties off its major blood vessels. Then the surgeon clamps the lung’s main bronchial (air) tube. The surgeon cuts through this tube as close to the trachea (windpipe) as possible. He or she then removes the lung.
The cut end of the bronchial tube either is closed with staples or tied off with sutures. The surgeon will confirm that the closed end of the bronchial tube is not leaking air. He or she will then close the chest incision with sutures. The surgeon will leave a temporary drain in the space between the two membranes that surround the lung.
If you are having an extrapleural pneumonectomy, the surgeon will remove your diseased lung. He or she also will carefully remove the pleura from your chest wall. Parts of your pericardium and diaphragm will be cut away on the affected side. These will be replaced with patches of Gore-Tex, a safe, synthetic material.
After your surgery, you will be taken to the surgical intensive care unit (ICU). For the first 24 hours, your breathing will be assisted with a respirator. Your chest drainage tube will remain in place.
Once your condition is stable, you will be transferred to a regular hospital room. This usually occurs within a few days.
Most patients who have had a traditional pneumonectomy will be able to go home seven to 10 days after their surgery. The hospital stay for an extrapleural pneumonectomy may be one or two days longer.
Many centers now offer less invasive surgery for selected candidates. This surgery is called video-assisted thoracic surgery (VATS). With VATS, the length of hospital stay may be reduced.
Follow-Up
Before you are discharged from the hospital, your surgeon will tell you when to return for your first follow-up visit. You will gradually resume your normal daily activities. As you do so, your remaining lung will slowly compensate for the loss of its partner.
Recovery tends to be slow for most people. Even six months after surgery, many pneumonectomy patients find that their ability to exercise is limited by shortness of breath.
Risks
Your thoracic surgeon will explain your personal risk. Short-term postoperative complications include:
- Dependence on a mechanical respirator for a prolonged period of time
- Heart problems, including cardiac arrhythmias and heart attack
- Pneumonia
- Wound infection
- A blood clot lodged in the lungs
- An abnormal connection between the stump of the cut bronchus and the pleural space
- Pus accumulation in the pleural space
- Fluid accumulation in the lungs
- Kidney failure
One long-term risk is shortness of breath. Some people may require oxygen. Oxygen can be administered at home, for many months or even years after the surgery.
When To Call A Professional
After your discharge, call your doctor immediately if:
- You develop chest pain, cough, or shortness of breath
- You have a fever
- Your incision becomes red, swollen and painful, or oozes blood
Additional Info
National Heart, Lung, and Blood Institute (NHLBI)
6701 Rockledge Drive
P.O. Box 30105
Bethesda, MD 20824-0105
Phone: (301) 592-8573
http://www.nhlbi.nih.gov/
National Cancer Institute (NCI)
Public Inquiries Office
Suite 3036A
6116 Executive Blvd., MSC 8322
Bethesda, MD 20892-8322
Phone: (301) 435-3848
Toll-Free: (800) 422-6237
http://www.nci.nih.gov/
American Cancer Society (ACS)
1599 Clifton Rd., NE
Atlanta, GA 30329-4251
Toll-Free: (800) 227-2345
http://www.cancer.org/
American Lung Association
1740 Broadway
New York, NY 10019
Phone: (212) 315-8700
Toll-Free: (800) 586-4872
http://www.lungusa.org/