Patient Basics: Tuberculosis
Originally published by Harvard Health.
What Is It?
Tuberculosis is a bacterial infection that kills more than 2 million people a year. Most of these deaths occur in developing countries. The bacterium that usually causes tuberculosis in humans is Mycobacterium tuberculosis.
About one-third of the world’s population is infected with tuberculosis. However, most do not show signs of the disease. In these people, the bacteria are inactive (latent) and cannot be transmitted to others. If the body’s immune system weakens, tuberculosis can become active and cause disease.
Worldwide, tuberculosis is second only to the human immunodeficiency virus (HIV) in causes of death by infectious disease among adults. Many developing countries are suffering dual epidemics of tuberculosis and HIV. The interaction between these two diseases has been labeled “Toxic synergy” because each epidemic impacts people in the same impoverished regions of the world, and because each worsens the other. People with HIV have weakened immune systems, so they are more likely to acquire a new case of tuberculosis, or to develop reactivation of latent disease. Those with tuberculosis are more likely to die if they are co-infected with HIV.
Tuberculosis typically affects the lungs. But in up to one-third of infected people, particularly those with HIV/AIDS, the illness also involves other areas of the body. Common sites of infection include the lymph nodes, the membranes that cover the brain (meninges), the joints, the kidneys and the membrane covering the digestive organs (peritoneum).
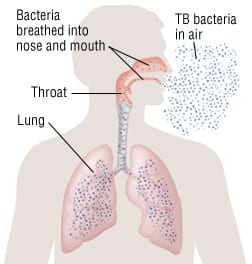
Tuberculosis bacteria are spread from person to person through the air. The bacteria are in droplets of secretions that come out of your mouth or nose when you cough or sneeze. One-time exposure to someone with tuberculosis is not likely to cause infection. Repeated or prolonged exposure is usually necessary. Touching someone with tuberculosis or sharing his or her utensils will not lead to infection, because the bacteria infect the lungs only when they are inhaled into the lungs.
When infection occurs, a bacteria-filled droplet is inhaled into the deepest portion of the lung, where the bacteria reproduce (replicate) and spread through the body. At this point, the immune system usually can keep the bacteria from replicating any more, but usually cannot destroy them completely. The disease usually remains in this inactive or dormant state for life. People with inactive tuberculosis do not have any symptoms, and there is no way to tell they have been infected except for a special skin test.
Active tuberculosis occurs in several different forms:
- Primary pulmonary tuberculosis – In about 5% of people, the immune system can’t stop the initial tuberculosis infection. These people develop active tuberculosis within one year of exposure to the bacteria. This type of active tuberculosis is most common in infants and children, especially in developing countries with high rates of malnutrition and poor medical care. People with HIV and other diseases that suppress the immune system are also at risk.
- Postprimary (reactivation) pulmonary tuberculosis – About 95% of people infected with tuberculosis can inactivate the disease at first. Most of them never develop active disease. In those that do, the bacteria eventually overcome the immune system and begin to replicate and spread, usually in the lungs. The bacteria may destroy large areas of the lungs, forming cavities filled with bacteria and dead cells.
- Extra-pulmonary tuberculosis – Tuberculosis also can become active in other parts of the body, whether or not the lungs are involved. Common sites of infection include the bones, kidneys, lymph nodes and central nervous system.
- Disseminated or miliary tuberculosis – Tuberculosis can spread through the entire body by way of the bloodstream.
Symptoms
Most people infected with tuberculosis have inactive disease that does not cause any symptoms. In these people, a skin test for tuberculosis (called a PPD skin test, for “protein purified derivative”) will show positive results within three months of getting the infection. Once a PPD is positive, it usually will remain positive throughout life.
Among people with active tuberculosis, symptoms vary according to the type of disease:
- Primary pulmonary tuberculosis – Some people, especially young children, with this type of tuberculosis have no symptoms other than fever and fatigue. Other symptoms can include:
- Cough
- Chest pain
- Night sweats
- Poor appetite
- Problems gaining weight
- Postprimary (reactivation) tuberculosis – Symptoms include:
- Fever
- Night sweats
- Weight loss
- Poor appetite
- Weakness
- Chest pain
- A general sick feeling
There usually is also a cough, which eventually produces discolored mucus. As the illness progresses, people may cough up blood (sometimes in large amounts), become short of breath and ultimately develop severe breathing problems.
- Extra-pulmonary tuberculosis – Symptoms depend on where the tuberculosis has spread. For example, if tuberculosis affects the lymph nodes (about 25% of cases), it can cause swollen glands, usually at the sides and base of the neck. In tuberculosis of the bones and joints (about 8% of cases), the spine, hips and knees are the most likely sites of infection. Joints will become painful and swollen. Genitourinary tuberculosis (about 15% of cases) can cause pain in the side (between the ribs and hip), frequent urination, pain or discomfort during urination, and blood in the urine.
- Disseminated or miliary tuberculosis – Symptoms include:
- Fever
- Night sweats
- Weight loss
- Weakness
- Lung problems (cough, shortness of breath, chest pain)
Although the bacteria are spread throughout the body, there may not be any other symptoms. But if there are, they can occur nearly anywhere. Some of the more common symptoms are:
- Headaches
- Visual difficulties
- Swollen lymph nodes
- Painful joints
- Scrotal masses
- Skin rashes
- Abdominal pain
Diagnosis
Your doctor will ask you about symptoms such as cough, fever, weight loss, night sweats, swollen glands and breathing problems. He or she also will ask whether you have ever been exposed to anyone with tuberculosis, and if you have ever traveled to developing countries where tuberculosis is common.
Your doctor will examine you. He or she will ask if you have ever had a tuberculosis skin test and what the results showed. If your doctor suspects that you have active pulmonary tuberculosis, he or she will have you get a chest X-ray. Your doctor will have you cough up samples of mucus (sputum), which will be stained with special chemicals and then examined for the presence of bacteria. The sputum also will be cultured, which means it is tested to see if tuberculosis bacteria grow. It may take up to several weeks to get the culture test result, because the bacteria grow slowly.
People with extra-pulmonary tuberculosis may have a normal chest X-ray and negative stains and cultures of their sputum. In these cases, other techniques are used to help make the diagnosis including:
- A blood test called QuantiFERON-Tb Gold
- Culture of other bodily fluids (such as urine or fluid from the space around the lung)
- Biopsy of tissue to look for characteristic changes consistent with TB
- Samples examined for evidence of tuberculosis using PCR (polymerase chain reaction)
Expected Duration
Once someone’s healthy immune system has controlled a primary tuberculosis infection, the bacteria usually will remain inactive for life. A PPD skin test may be positive in these people, indicating a history of tuberculosis infection, but the lifetime chance of developing active TB disease is only about 10%, unless your immune system is weakened by a disease such as HIV/AIDS or medications that suppress the immune system.
If you develop active tuberculosis disease, it takes up to two weeks of treatment before you can no longer spread tuberculosis to other people. However, it takes at least six months to complete successful treatment. In some cases, patients are infected with strains of tuberculosis that are resistant to the most commonly used and effective antibiotics. These resistant strains can take up to 24 months to treat.
Prevention
In developing countries with high rates of tuberculosis, a vaccine against the disease often is given at birth. The vaccine is not used routinely in the United States and most European countries because the risk of transmission in these countries is low, and because the vaccine is not very effective.
People with a positive skin test for TB (PPD) who have never received medication to prevent TB from becoming active should consider taking isoniazid (INH) for up to 9 months. Also people with HIV infection who live in parts of the world that have high rates of TB are encouraged to take isoniazid, even if they have a negative PPD.
Treatment
Doctors usually treat tuberculosis with a combination of four drugs, such as isoniazid (INH), rifampin (Rifadin, Rimactane), pyrazinamide (pms-Pyrazinamide, Tebrazid) and ethambutol (Myambutol). This combination is considered first line treatment. The therapy usually lasts 6 months or longer. It is very important that you take these medications as prescribed to prevent the bacteria from becoming resistant to the drugs. It is also important that all of your close contacts are screened for tuberculosis, so they can be treated if they are infected.
Tuberculosis strains that are resistant to isoniazid and rifampin (the two most effective tuberculosis antibiotics) are called multidrug resistant (MDR-TB). To cure MDR-TB, patients must take combinations of “second-line” tuberculosis medications: ethionamide (Trecator-SC), moxifloxacin (Avelox), levofloxacin (Levaquin), cycloserine (Seromycin), kanamycin (Kantrex) and others. These medications are more likely to cause side effects than first-line drugs are. Also they are not as effective so they must be taken for up to two years.
Extensively drug-resistant (XDR-TB) strains have been identified in many countries throughout the world. These strains are resistant to isoniazid, rifampin, the aminoglycoside drug family (such as kanamycin), and the quinolone drug family (such as levofloxacin and moxifloxacin). XDR-TB is very difficult to treat, and sometimes, surgery is necessary to remove the diseased portion of the lung.
In the past, it was felt that drug-resistant TB was incurable in the developing world because the second-line drugs were too expensive, costing up to $15,000 per person per year. Now these drugs can be obtained through the World Health Organization (WHO) for as little as 5% of the prior cost. Treatment programs have been started in most developing nations.
When To Call a Professional
Call your doctor if you develop cough, fever, weight loss, swollen glands, night sweats or other symptoms of tuberculosis. You also should call your doctor if you have been exposed to someone with active tuberculosis. Ask your doctor about your need for routine PPD testing if you often travel to developing countries or work in an environment where tuberculosis risk is high, such as a medical facility or institution.
Prognosis
Tuberculosis that is not resistant to medication is almost always cured if the person complies with the treatment regimens and antibiotics are started before major parts of the lung are destroyed. People who are infected with drug-resistant tuberculosis strains may have less chance of being cured, depending on which drugs they are resistant to and how much lung damage they have before effective treatment is started.
Without proper treatment, more than half of people with active tuberculosis will die within five years.
Additional Info
National Institute of Allergy and Infectious Diseases (NIAID)
Office of Communications & Public Liaison
6610 Rockledge Drive, MSC6612
Bethesda, MD 20892-6612
Phone: 301-496-5717
Toll-Free: 1-866-284-4107
TDD: 1-800-877-8339
http://www.niaid.nih.gov/
American Lung Association
61 Broadway, 6th Floor
New York, NY 10006
Phone: 212-315-8700
Toll-Free: 1-800-548-8252
http://www.lungusa.org/
World Health Organization (WHO)
Avenue Appia 20
1211 Geneva 27
Switzerland
Phone: + 41 22 791 21 11
Fax: + 41 22 791 31 11
http://www.who.int/