Pembrolizumab did not show overall survival benefit in patients with microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer
1. The median overall survival for pembrolizumab versus chemotherapy was not statistically significant difference.
2. Common grade 3 or higher treatment-related adverse events in patients receiving pembrolizumab were diarrhea, fatigue, and anemia.
Evidence Rating Level: 1 (Excellent)
Study Rundown: The presence of mismatch repair deficiency in colorectal cancer can help inform the surgical and systemic treatment for patients. Based on the initial data from the KEYNOTE-177 study, pembrolizumab showed improved progression-free survival compared to chemotherapy in patients with previously untreated microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer. This study presents the final overall survival analysis of the KEYNOTE-177 study. At final analysis, the median overall survival as per the intention-to-treat analysis was not statistically different. Diarrhea, fatigue, and anemia were common grade 3 or higher treatment-related adverse events that were reported. It is important to note that the crossover design could have contributed to the absence of significant overall survival benefit for pembrolizumab. 36% of the patients in the chemotherapy group crossed over to receive pembrolizumab and 24% received off-study anti-PD-1/anti-PD-L1 therapies. The high cross-over rate could have contributed to an improvement in the overall survival rate in the chemotherapy group. Overall, this study demonstrated that although prior reported analysis indicated a large progression-free survival benefit and quality of life benefits, the overall survival was not different likely owing to substantial cross-over and off-label use of immunotherapy.
Click to read the study in The Lancet Oncology
Relevant Reading: Pembrolizumab in microsatellite instability-high advanced colorectal cancer
In-Depth [randomized controlled trial]: This was an open label, randomized, phase III study. Patients were eligible if they had previously untreated microsatellite instability-high or mismatch repair-deficient metastatic colorectal cancer. Patients who have received adjuvant therapy for colorectal cancer 6 months prior to randomization were also included. A total of 307 patients were enrolled to receive either study treatment (n=153) or chemotherapy (n=154). Patients whose disease progressed while receiving chemotherapy were allowed to cross over to pembrolizumab for up to 35 treatment cycles. At data-cutoff, 36% of the patients in the chemotherapy group crossed over to receive pembrolizumab in the intention-to-treat group. The demographic of both study groups was well-balanced. The median follow-up period was 44.5 months (interquartile range [IQR]: 39.7-49.8). The median overall survival for pembrolizumab (median not reached [NR], 95% confidence interval [CI]: 49.2-NR) versus chemotherapy (median 36.7 months, 95% CI: 27.6-NR) did not show statistical difference. Treatment-related adverse events for Grade 3 or worse occurred in 22% of the pembrolizumab group versus 66% in the chemotherapy group. These included diarrhea (2%), fatigue (2%), and anemia (1%) in the pembrolizumab group. In addition, there was no treatment-related death in the pembrolizumab group.
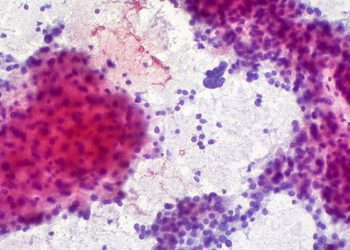
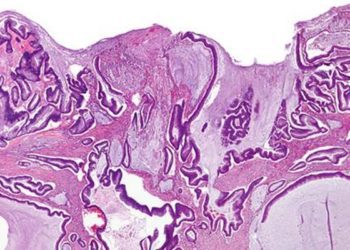
Image: PD
©2022 2 Minute Medicine, Inc. All rights reserved. No works may be reproduced without expressed written consent from 2 Minute Medicine, Inc. Inquire about licensing here. No article should be construed as medical advice and is not intended as such by the authors or by 2 Minute Medicine, Inc.